Pattern of antimicrobial prescription in Africa: a systematic review of point prevalence surveys
Ijeoma Nkem Okedo-Alex, Ifeyinwa Chizoba Akamike, Ihoghosa Iyamu, Chukwuma David Umeokonkwo
Corresponding author: Ijeoma Nkem Okedo-Alex, Department of Community Medicine, Alex Ekwueme Federal University Teaching Hospital, Abakaliki Ebonyi State, Abakaliki, Nigeria 
Received: 04 Jul 2022 - Accepted: 23 Apr 2023 - Published: 29 May 2023
Domain: Infectious diseases epidemiology,Global health,Public health
Keywords: Antibiotics, antimicrobial, prescription, point prevalence, survey, Africa, systematic review
©Ijeoma Nkem Okedo-Alex et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Ijeoma Nkem Okedo-Alex et al. Pattern of antimicrobial prescription in Africa: a systematic review of point prevalence surveys. Pan African Medical Journal. 2023;45:67. [doi: 10.11604/pamj.2023.45.67.36191]
Available online at: https://www.panafrican-med-journal.com//content/article/45/67/full
Review 
Pattern of antimicrobial prescription in Africa: a systematic review of point prevalence surveys
Pattern of antimicrobial prescription in Africa: a systematic review of point prevalence surveys
![]() Ijeoma Nkem Okedo-Alex1,2,&,
Ijeoma Nkem Okedo-Alex1,2,&, ![]() Ifeyinwa Chizoba Akamike1,2, Ihoghosa Iyamu3,4,
Ifeyinwa Chizoba Akamike1,2, Ihoghosa Iyamu3,4, ![]() Chukwuma David Umeokonkwo1
Chukwuma David Umeokonkwo1
&Corresponding author
Introduction: inappropriate use of antimicrobials is a cause for concern and contributes to the global antimicrobial resistance crises especially in Africa. This review aims to summarize the available evidence on the point prevalence and pattern of antimicrobial and/or antibiotic prescription in Africa.
Methods: this review was carried out between April and September 2021 and identified published studies up until March 2021 on the point prevalence of antibiotic and/or antimicrobial use in Africa. Sources searched were OVID, PubMed, EMBASE, CINAHL, Web of Science, Google Scholar, Google, and African Journal Online (AJOL). Observational studies that reported prevalence published in English language were included. Covidence systematic review software was used for this review. A form for data extraction using domains culled from the Global Point Prevalence Survey of Antimicrobial Consumption and Resistance (Global-PPS) was developed on Covidence. Screening of studies for eligibility was done independently by two reviewers. Critical Appraisal tool for use in Joanna Briggs Institute (JBI) Systematic Reviews for prevalence studies was used for quality appraisal.
Results: a total of 17 studies that met the inclusion criteria were included in the review. The overall prevalence of antimicrobial/antibiotic use among inpatients in these studies ranged from 40.7% to 97.6%. The median antimicrobial/antibiotic use was 61.3 [IQR= 45.5-72.1]. The highest use of antimicrobials was reported among studies from Nigeria with a prevalence of 97.6%. The most prescribed antibiotics were the beta-lactam penicillin (Amoxicillin, clavulanic acid) (86.9%), and third generation cephalosporins (55.0%). There was general preference for parenteral route of administration of the antimicrobial agents (40-70%). Use for community acquired infections (28.0-79.5%) was the main reason for use. Majority of the prophylactic use of antimicrobial agents was for surgical prophylaxis.
Conclusion: the high prevalence of antimicrobial use in Africa reinforces the need for continued surveillance and concerted efforts to institutionalize and support antimicrobial stewardship for prescribers in health institutions in the African region.
Antimicrobials are important agents in reducing morbidity and mortality among patients who have infections, however, the frequent inappropriate and excessive use of antimicrobials is a cause for concern because of the risk of antimicrobial resistance [1-3]. Factors that contribute to the global AMR crises include overprescribing and over-dispensing of antimicrobial drugs by health workers, patient noncompliance with therapy, poor quality medicines, wrong prescription and dosage, and poor infection prevention and control practices [4]. The highest AMR burden is seen in low and middle income-countries including countries in Africa. A range of activities and programs to enhance appropriate antibiotic prescribing ranging from global, regional and national levels have been carried out as a result of the concerns with the increasing rate of AMR. In response to the AMR crises, the World Health Organization (WHO) developed a Global Action Plan (GAP), with a goal to ensure the successful treatment and prevention of infectious diseases using effective and safe medicines that are quality-assured. These medicines are to be used in a responsible way, and expected to be accessible to all who need them [5]. Point prevalence survey (PPS) is a necessary means of providing accurate data on the current antibiotics utilization [6,7]. It provides information that can be used to improve antimicrobial use in hospitals and thereby reduce resistance [6,7]. Additionally, it can be used to monitor antimicrobial stewardship and infection control programs. The aim of developing the WHO PPS methodology [8] was to collect baseline information on antibiotics use in hospitals. This information is collected from medical records and other associated patient records relevant for treatment and management of infectious diseases and is expected to be repeated once every few years [4]. The specific objectives of the methodology include providing a standardized methodology which can be used to estimate the prevalence of antibiotics use in hospitals and provide information on prescribing patterns; and also make available information for decision making by policy makers [4]. Although, several PPS studies have reported varying prevalence of antibiotics use and provided insight into current antibiotic prescribing practices, there is a dearth of evidence synthesis on this subject in Africa [7,9-12]. This review aims to summarize the available evidence on the point prevalence and pattern of antimicrobial and/or antibiotic prescription in Africa in order to identify areas for improvement and inform future policies.
For screening eligible studies, this review utilized the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [PRISMA] checklist for reporting a systematic review or meta-analysis protocol [13].
Protocol registration : the protocol can be found at [14] with registration number: CRD42020215879 [14].
Search strategy : this review was carried out between April and September 2021 and identified published studies up until March 2021 on the point prevalence of antibiotic and/or antimicrobial use in Africa. The following databases and sources were searched: OVID, PubMed, EMBASE, CINAHL, Web of Science, Google scholar, Google, and African journal online (AJOL). Some of the terms employed in the search include but are not limited to the following: prevalence, point prevalence, antibiotic, antimicrobial, prescription use, Africa. The search strategy is contained in (Annex 1, Annex 2).
Inclusion criteria: the eligibility criteria for inclusion of studies include cross-sectional studies regardless of publication period published or retrievable in English language, and studies conducted in Africa. The study must report point prevalence of antimicrobial/antibiotic prescription or use in health care settings using point prevalence survey tools.
Exclusion criteria: the studies excluded were those not published in English language, multi-country studies, reviews, editorials, commentaries, case reports, case series and qualitative.
Data extraction: the authors utilized the Covidence systematic review software for this review [15]. Two of the reviewers (INO and ICA) independently screened the titles and abstracts and all the reviewers were involved in data extraction from the full texts. The Covidence software automatically kept track of consensus and conflicts which were resolved by discussions. References of the published studies were managed using the Mendeley reference manager. The reviewers jointly developed a form for data extraction on Covidence using domains culled from the Global Point Prevalence Survey of Antimicrobial Consumption and Resistance (Global-PPS) [16]. Some of the fields in the extraction form were first author´s name, year the study was conducted, year the study was published, study location and setting, country of study, title/objective, study design, sample size, prevalence type (antibiotic/antimicrobial), prevalence of antibiotic/antimicrobial use (for studies involving multiple sites with no reported overall prevalence, the average value was taken as the overall prevalence), prevalence of most used antibiotic, prevalence of least used antibiotic, route and indication for use, stop/review dates etc. The process through which the articles were selected and included is shown in Figure 1.
Quality appraisal: all reviewers participated in the quality appraisal process which was done using the Critical Appraisal tools for use in JBI Systematic Reviews tool for prevalence studies [17] (Annex 3). This quality assessment tool contained nine questions which explored the adequacy of the sample frame, sampling of study participants, adequacy of sample size, description of study subjects and setting, data analysis conducted with sufficient coverage of the identified sample, use of valid methods used for the identification of the condition, response rate and appropriate statistical analysis amongst others. A final assessment to include or exclude was also part of this tool. For each variable, the options to score from were Yes, No, Unclear, and not applicable. The adequacy of the sample size was not applicable to any of the studies included in this review as sample size calculation is not required by the PPS tool. For the other parameters, all the seventeen studies that fulfilled the inclusion criteria were scored "Yes" and a final decision was made to include them in the study.
Patient and public involvement: it was not appropriate nor possible to involve patients or the public in this work.
Among 1356 studies returned in our database search, 505 duplicates were identified and removed. Further, 812 studies were excluded during the title and abstract review, resulting in thirty-nine full texts being assessed for eligibility. Of these, nine were removed because the study was not relevant to the study objective, ten removed because there were review articles or they were multi-country studies and three were excluded because they were either only abstract or the full text were not available. A total of 17 studies were included in the review. A total of 17 articles [6,7,9-11,18-29] published between 2017 and 2021 were included in the review. The studies were all cross-sectional design using mostly the global PPS, WHO PPS or ECDC PPS tools (Table 1). Five studies were conducted in Nigeria, four from Ghana, three from Kenya, two from South Africa and Tanzania respectively and one from Benin. The studies were conducted in West, Central and South African region involving over 14,000 patients (Table 1). The overall prevalence of antimicrobial/antibiotic use among inpatients in these studies ranged from 40.7% to 97.6%. Nigeria had the highest prevalence (97.6%) while South Africa had the lowest prevalence of antimicrobial/antibiotic use (37.7%). The median antimicrobial/antibiotic use was 61.3% (interquartile range [IQR] (45.5-72.1). The most prescribed antibiotics were the beta-lactam penicillin (Amoxicillin, clavulanic acid) (86.9%), and third generation cephalosporins (55.0%). The second most-used antimicrobial apart from cephalosporins (44.7%) was nitroimidazoles/metronidazole (41.8%) (Table 2).
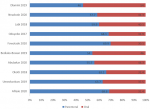
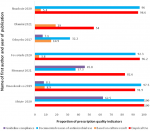
The majority of the studies (10/17, 58.8%) reported the route of administration of the antimicrobial agent used. There was general preference for parenteral route of administration of the antimicrobial agents (40-70%) (Figure 2). The indication for use of antibiotics was reported in majority of the studies. Regarding the therapeutic indications, most reasons for the use of antibiotics were for community-acquired infections (28.0-79.5'5%). Some studies also reported significant proportion of the prescriptions were for hospital-acquired infections (19.1-30.8%). The majority of the prophylactic use of antimicrobial agents were for surgical prophylaxis (Table 3). However, some significant use for medical prophylaxis were also reported (15;5.1-40.9%). Some studies also reported some therapeutic and prophylactic use of antimicrobial agents for which there was no clear diagnosis. There were variations in reporting prescription quality indicators due to the focus of the studies and the type of tools they employed. Among the studies that reported prescription quality indicators, there was wide variations in the proportion reported. Most studies reported poor utilization of laboratories in making bacteriological diagnosis of infection as most antimicrobial prescription were done in empirical basis. It was also evident that there was little or no guidelines available in most of the studies settings. Where guidelines were available for antibiotic prescription, these were largely not complied with (0%-62.5'5%) (Figure 3).
In this systematic review of publications assessing the prescription pattern and use of antimicrobials based on the various forms of the PPS methodology in Africa, we found a generally high prevalence of antimicrobial prescription and use. We also found considerable variation in antimicrobial use among studies from various countries, with Nigeria having the highest prevalence of antimicrobial use and Benin and South Africa reporting the lowest prevalence of antimicrobial use. Further, we found that the most prescribed antibiotics were third generation cephalosporins, beta-lactam penicillin and the Nitroimidazoles (including metronidazole). This review also showed that the most common indications for antimicrobials were for community acquired infections and for prophylaxis in surgical and medical cases. Our systematic review provides an in-depth understanding about antimicrobial prescription and use patterns in Africa. First, unlike previous studies which suggested limited use of the PPS methodology in Africa, we found 17 studies using various versions of the methodology, suggesting increasing concerns about tracking antimicrobial use which is a key strategy in the global action plan an antimicrobial stewardship [5]. The high prevalence of antimicrobial use found in our study is similar with other global studies that highlight inappropriate use of antimicrobials in the region as a global health problem [30]. However, the prevalence of antimicrobial use in this study was relatively higher than reported in other regions of the world including Europe and North America [30,31]. Studies have found higher antimicrobial stewardship levels and awareness of antimicrobial use among prescribers in South Africa and this could explain the lower levels of antimicrobial use compared to other countries [32,33].
The variation in antimicrobial prescription may be due to varied existence and adherence to antimicrobial prescription guidelines including a large dependence on empirical basis for prescription, variations in prevalence of infectious diseases (including community- and hospital-acquired infections) and sub-standard infection prevention and control practices in hospitals [30]. Further, our findings of broad-spectrum antibiotics including third generation cephalosporins and beta-lactam penicillin suggests that clinicians may be adopting empirical use of broad-spectrum antibiotics as a strategy to manage infections in jurisdictions where access to diagnostic services including microbial culture and susceptibility testing may be limited [30,34]. It could also reflect rising rates of multi-drug antimicrobial resistance which have been documented as having a significant burden in low- and middle-income countries including those in Africa [34].
The findings from our systematic review are of clinical and global health importance considering the rising threat and burden of antimicrobial resistance in the region. Systematic misuse and overuse of antimicrobials among human populations, especially in-hospital settings continue to contribute significantly to the global health threat of antimicrobial resistance [34,35]. Findings from our systematic review suggest that there is need for sustainable antimicrobial stewardship programs with standardized antimicrobial prescription guidelines within health systems in the region. For optimal adherence, it is also important that there is strengthened capacity-building among clinicians in the region, ensuring that these guidelines and minimum standards that enable good institutional antimicrobial prescription practices are adhered to. Optimal infection prevention and control practices can also motivate correct antimicrobial prescription especially for prophylaxis [35]. However, we must note that challenges regarding care provider-patient interactions only contribute a fraction to the issues, as there are concerns about the quality of antimicrobials that also influence prescription behavior [35].
Findings from this study should be considered in view of its inherent limitations. Firstly, the variety of the tools, varied types of prevalence reported (antimicrobial/antibiotic) as well as different patient populations targeted by the included papers implied that we were unable to make comparisons between the studies and their varied jurisdictions due to the non-equivalence of some of their findings. Further, our study only included articles published in English. Considering that some articles from Africa may have been published in French, this may introduce some bias into this review. However, given the observed trends in the data, we are confident that our review is sufficient to demonstrate the current state of antimicrobial prescription and use on the continent.
Our study demonstrates the utility of the PPS tools to assess the prevalence and patterns of antimicrobial use within hospitals, providing a basis for quality improvement in line with the WHO GAP on antimicrobial stewardship. The high prevalence of antimicrobial use in sub-Saharan Africa reinforces the need for continued surveillance and concerted efforts to institutionalize and support antimicrobial stewardship for prescribers in health institutions in the region.
What is known about this topic
- Antimicrobial resistance is a growing concern globally;
- Point prevalence surveys have been useful in describing the use of antimicrobials and health facilities.
What this study adds
- There review showed a high prevalence of antimicrobial prescription across African regions and countries;
- Parenteral administration, surgical prophylaxis, empirical basis and antimicrobial use for community-acquired infections are prevalent in African health settings.
The authors declare no competing interests.
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All the authors read and approved the final version of the manuscript.
Table 1: characteristics of studies included in the review
Table 2: prevalence and pattern of antimicrobial/antibiotic use
Table 3: indication for use of antimicrobial agents
Figure 1: prisma diagram showing the process of selection and inclusion of studies
Figure 2: distribution of route of antimicrobial administration among the studies
Figure 3: distribution of prescription quality indicators reported among the studies
Annex 1: PRISMA checklist for reporting a systematic review or meta-analysis protocol (PDF-395 ko)
Annex 2: search strategy for the systematic review on the point prevalence and pattern of antimicrobial prescription in Africa (PDF-396 ko)
Annex 3: quality appraisal tools for studies included in the systematic review on the point prevalence and pattern of antimicrobial prescription in Africa (PDF-408 ko)
- Laxminarayan R, Matsoso P, Pant S, Brower C, Røttingen J-A, Klugman K et al. Access to effective antimicrobials: a worldwide challenge. Lancet. 2016;387(10014):168-75. PubMed | Google Scholar
- O´Neill J. Securing new drugs for future generations: the pipeline of antibiotics. The review of antimicrobial resistance. 2015.
- Founou R, Founou L, Essack S. Clinical and economic impact of antibiotic resistance in developing countries: a systematic review and meta-analysis. PLoS One. 2017;12:e0189621. PubMed | Google Scholar
- World Health Organization. World Health Organization methodology for Point Prevalence Survey on Antibiotic Use in Hospitals. World Health Organization.2018. Google Scholar
- World Health Organization. Global action plan on antimicrobial resistance. World Health Organization. 2015. Google Scholar
- Kruger D, Dlamini NN, Meyer JC, Godman B, Kurdi A, Lennon M et al. Development of a web-based application to improve data collection of antimicrobial utilization in the public health care system in South Africa. Hosp Pract. 2021 Aug;49(3):184-193. PubMed | Google Scholar
- Horumpende PG, Mshana SE, Mouw EF, Mmbaga BT, Chilongola JO. Point prevalence survey of antimicrobial use in three hospitals in North-Eastern Tanzania: antimicrob resist Infect control. Antimicrobial Resistance & Infection Control. 2020 Sep 7;9(1):149. PubMed | Google Scholar
- World Health Organization. World Health Organization methodology for Point Prevalence Survey on Antibiotic Use in Hospitals. World Health Organization. 2018. Google Scholar
- Seni J, Mapunjo SG, Wittenauer R, Valimba R, Stergachis A, Werth BJ et al. Antimicrobial use across six referral hospitals in Tanzania: a point prevalence survey. BMJ Open. 2020;10(12):e042819. PubMed | Google Scholar
- Momanyi L, Opanga S, Nyamu D, Oluka M, Kurdi A, Godman B. Antibiotic prescribing patterns at a Leading Referral Hospital in Kenya: a point prevalence survey. J Res Pharm Pr. 2019;8(3):149-54. PubMed | Google Scholar
- Ahoyo TA, Bankolé HS, Adéoti FM, Gbohoun AA, Assavèdo S, Amoussou-guénou M et al. Prevalence of nosocomial infections and anti-infective therapy in Benin: results of the first nationwide survey in 2012. Antimicrob Resist Infect Control. 2014;3:17. PubMed | Google Scholar
- Paramadhas BDA, Tiroyakgosi C, Mpinda-joseph P, Morokotso M, Matome M, Sinkala F et al. Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Expert Rev Anti Infect Ther. Taylor & Francis; 2019;17(1):535-46. PubMed | Google Scholar
- Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647. PubMed | Google Scholar
- Okedo-Alex IN, Akamike IC, Iyamu I, Umeokonkwo CD. Protocol for systematic review on pattern of antimicrobial prescription in Africa: a systematic review of point prevalence surveys. 2021.
- Veritas Health Innovation. Covidence systematic review software. Melbourne, Australia: Veritas Health Innovation. Google Scholar
- University of Antwerp. The Global Point Prevalence Survey of antimicrobial consumption and resistance (Global-PPS). 2006. Google Scholar
- Joanna Briggs Institute. JBI´s critical appraisal tools: Checklist for Analytical Cross Sectional Studies. Crit Apprais tools download. Google Scholar
- Afriyie DK, Sefah IA, Sneddon J, Malcolm W, McKinney R, Cooper L. Antimicrobial point prevalence surveys in two Ghanaian hospitals: opportunities for antimicrobial stewardship. JAC-Antimicrobial Resist. 2020 Feb 18;2(1):dlaa001. PubMed | Google Scholar
- Umeokonkwo CD, Madubueze UC, Onah KC, Okedo-Alex IN, Adeke SA, Versporten A et al. Point prevalence survey of antimicrobial prescription in a tertiary hospital in South East Nigeria: a call for improved antibiotic stewardship. Integr Med Res Taibah University. 2019;17:291-5. PubMed | Google Scholar
- Maina M, Mwaniki P, Odira E, Kiko N, McKnight J, Schultsz C et al. Antibiotic use in Kenyan public hospitals: prevalence, appropriateness and link to guideline availability. International Society for Infectious Diseases. 2020;99:10-8. PubMed | Google Scholar
- Okoth C, Opanga S, Okalebo F, Oluka M, Baker Kurdi A, Godman B. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: findings and implications. Hosp Pract (1995) Taylor & Francis. 2018;46(3):128-36. PubMed | Google Scholar
- Bediako-bowan AAA, Owusu E, Labi A, Obeng-Nkrumah N, Sunkwa-Mills G, Bjerrum S et al. Antibiotic use in surgical units of selected hospitals in Ghana: a multi-centre point prevalence survey. BMC Public Health. 2019;19(1):797. PubMed | Google Scholar
- Fowotade A, Fasuyi T, Aigbovo O, Versporten A, Adekanmbi O, Akinyemi O et al. Point prevalence survey of antimicrobial prescribing in a Nigerian Hospital: findings and implications on antimicrobial resistance. West Afr J Med Nigeria. 2020;37(3):216-20. PubMed | Google Scholar
- Oduyebo O, Olayinka A, Iregbu K, Versporten A, Goossens H, Nwajiobi-Princewill P et al. A point prevalence survey of antimicrobial prescribing in four Nigerian tertiary hospitals. Ann Trop Pathol. 2017;8(1):42-6. Google Scholar
- Labi A-K, Obeng-Nkrumah N, Owusu E, Bjerrum S, Bediako-Bowan A, Sunkwa-Mills G et al. Multi-centre point-prevalence survey of hospital-acquired infections in Ghana. J Hosp Infect England;.2019;101(1):60-8. PubMed | Google Scholar
- Labi A-K, Obeng-Nkrumah N, Nartey ET, Bjerrum S, Adu-Aryee NA, Ofori-Adjei YA et al. Antibiotic use in a tertiary healthcare facility in Ghana: a point prevalence survey. Antimicrob Resist Infect Control. 2018;7:15. PubMed | Google Scholar
- Nnadozie U, Umeononkwo C, Maduba C, Igwe-Okomiso D, Onah C, Madubueze U et al. Antibiotic use among surgical inpatients at a tertiary health facility; a case for a statandardized protocol for presumptive antimicrobial therapy in the developing world. infection prevention in practice. 2020 Jul 28;2(4):100078. PubMed | Google Scholar
- Dlamini NN, Meyer JC, Kruger D, Kurdi A, Godman B, Schellack N. Feasibility of using point prevalence surveys to assess antimicrobial utilisation in public hospitals in South Africa: a pilot study and implications. Hosp Pract (1995). 2019 Apr;47(2):88-95. PubMed | Google Scholar
- Abubakar U. Antibiotic use among hospitalized patients in northern Nigeria: a multicenter point-prevalence survey. BMC Infectious Diseases. 2020;20(1):86. PubMed | Google Scholar
- Saleem Z, Hassali MA, Godman B, Versporten A, Hashmi FK, Saeed H et al. Point prevalence surveys of antimicrobial use: a systematic review and the implications. Expert Rev Anti Infect Ther. 2020;18(9):897-910. PubMed | Google Scholar
- Selcuk A. The point prevalence and inappropriateness of antibiotic use at hospitals in Turkey: a systematic review and meta-analysis. J Chemother Taylor & Francis. 2021;33(6):390-9. PubMed | Google Scholar
- Elton L, Thomason MJ, Tembo J, Velavan TP, Pallerla SR, Arruda LB et al. Antimicrobial resistance preparedness in sub-Saharan African countries. Antimicrob Resist Infect Control. 2020;9(1):145. PubMed | Google Scholar
- Fasina FO, LeRoux-Pullen L, Smith P, Debusho LK, Shittu A, Jajere SM et al. Knowledge, attitudes, and perceptions associated with antimicrobial stewardship among veterinary students: a multi-country survey from Nigeria, South Africa, and Sudan. Front Public Heal. 2020 Oct 21;8:517964. PubMed | Google Scholar
- Tadesse BT, Ashley EA, Ongarello S, Havumaki J, Wijegoonewardena M, González IJ et al. Antimicrobial resistance in Africa: a systematic review. BMC Infectious Diseases. 2017;17(1):616. PubMed | Google Scholar
- Ayukekbong JA, Ntemgwa M, Atabe AN. The threat of antimicrobial resistance in developing countries: causes and control strategies. Antimicrobial Resistance & Infection Control. 2017;6:47. PubMed | Google Scholar