Cerebral ischemia, a rare postoperative complication of cervical disc herniation: a case report
Dahmane Elhairech, Mohamed Lmejatti
Corresponding author: Dahmane Elhairech, Neurosurgery Department, Hassan II University Hospital, Agadir City, Morocco 
Received: 28 May 2023 - Accepted: 01 Feb 2025 - Published: 07 Mar 2025
Domain: Neurology (general),Neuroradiology,Vascular Neurology
Keywords: Cervical hernia, ischemic stroke, surgery, medical treatment, case report
©Dahmane Elhairech et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Dahmane Elhairech et al. Cerebral ischemia, a rare postoperative complication of cervical disc herniation: a case report. Pan African Medical Journal. 2025;50:67. [doi: 10.11604/pamj.2025.50.67.40590]
Available online at: https://www.panafrican-med-journal.com//content/article/50/67/full
Case report 
Cerebral ischemia, a rare postoperative complication of cervical disc herniation: a case report
Cerebral ischemia, a rare postoperative complication of cervical disc herniation: a case report
&Corresponding author
Cervical spondylotic myelopathy is a degenerative disease that often requires surgical intervention. Postoperative cerebral ischemia is a rare but serious complication of cervical disc herniation surgery, with its pathophysiology poorly described. Intraoperative carotid manipulation is the most likely cause of this ischemia. We report a case of ischemic stroke as a complication following cervical disc herniation surgery in a 52-year-old patient. The patient developed left hemiplegia and central facial palsy immediately after surgery. Imaging revealed an ischemic stroke in the right Sylvian territory associated with atherosclerotic changes in the right common carotid artery. Early postoperative rehabilitation and antiplatelet therapy led to partial recovery. This case highlights the importance of careful carotid management during surgery and the need for preoperative assessment in high-risk patients.
Cervical disc herniation is a common degenerative disorder often requiring surgical intervention. While surgery is generally successful, it can be complicated by a range of postoperative events. Among these, cerebral ischemia is a rare but serious complication, occurring in only 0.22% of cases. The pathophysiology of postoperative cerebral ischemia following cervical disc herniation surgery is not well understood but is believed to be primarily linked to intraoperative manipulation of the carotid artery. As cervical degenerative disorders increasingly affect a younger population, understanding these risks becomes crucial. This report presents a case of ischemic stroke as a postoperative complication of cervical disc herniation surgery in a 52-year-old patient, aiming to raise awareness of the potential vascular risks associated with such procedures.
Patient information: a 52-year-old male patient with no significant medical history presented with cervico-brachial neuralgia radiating to the left anterior arm. This symptom persisted for three months and was resistant to medical treatment.
Clinical findings: on clinical examination, pyramidal signs were noted in all four limbs, along with intermittent claudication.
Timeline of current episode: symptoms of cervico-brachial neuralgia developed over the last three months, and the patient underwent surgery shortly after a diagnosis of cervical disc herniation at C3-C4 and C4-C5.
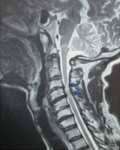
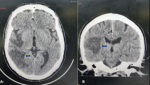
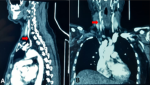
Diagnostic assessment: cervical Magnetic resonance imaging (MRI) revealed disc herniations at the C3-C4 and C4-C5 levels, with thinning of the anterior peri-medullary space (Figure 1). Postoperatively, a cerebral Computed Tomography (CT) scan without contrast injection in the axial and coronal sections showed right temporo-parietal hypodensity in favor of ischemic stroke in the Sylvian territory (Figure 2 A,B). Angioscan of the neck vessels in the sagittal and coronal sections revealed an atherosclerotic plaque of the right common carotid artery (Figure 3).
Diagnosis: ischemic stroke associated with intraoperative carotid manipulation during cervical disc herniation surgery.
Therapeutic interventions: the patient underwent anterior discectomy with cervical cage and plate fixation. Postoperatively, the patient developed left hemiplegia and central facial palsy. Antiplatelet therapy was initiated, alongside motor rehabilitation.
Follow-up and outcome of interventions: after one year, the patient maintained some degree of left hemiparesis but retained walking autonomy.
Patient perspective: the patient expressed relief from his initial symptoms of neuralgia but acknowledged the significant impact of the stroke on his quality of life.
Informed consent: it was obtained from the patient and his family for the publication of this case report.
Epidemiology: cerebral ischemia following cervical disc herniation surgery is a rare but serious complication. It highlights the potential risks associated with the manipulation of cervical arteries during surgery. Several risk factors may increase the likelihood of ischemic events, including advanced age, a history of atherosclerotic disease, and prior surgical history [1-4]. Although this complication is uncommon, it becomes more significant as the population undergoing cervical disc surgery includes individuals with multiple comorbidities and atherosclerotic changes.
Diagnosis: the diagnosis of postoperative cerebral ischemia is typically based on imaging studies, with cerebral computed tomography (CT) being the first-line investigation to identify ischemic changes in the brain. In this case, the brain scan revealed a right temporo-parietal hypodensity, indicating ischemia in the Sylvian territory, which confirmed the diagnosis of ischemic stroke [2,4,5]. Magnetic resonance imaging (MRI) may also be utilized in further evaluation to better assess the extent and location of the ischemic lesion.
Treatment: postoperative management for ischemic stroke typically involves antiplatelet therapy or anticoagulation, depending on the timing of the ischemic event. Thrombolytic therapy with tissue plasminogen activators (tPA) may be considered if the stroke occurs within the first few hours of onset, but it is contraindicated in the first 14 days after neurological surgery due to the risk of hemorrhage [4,6]. In this case, the patient was treated with antiplatelet therapy and motor rehabilitation, which significantly contributed to their recovery. The timely initiation of rehabilitation was key to maintaining functional independence.
Prognosis: the long-term prognosis for patients who experience cerebral ischemia after cervical disc herniation surgery can vary based on the severity and location of the ischemic lesion. In this case, the patient maintained walking autonomy but continued to experience hemiparesis. Early recognition and intervention, such as the use of antiplatelet therapy and motor rehabilitation, played a crucial role in preventing further neurological deterioration. Despite some residual deficits, the patient was able to regain a level of independence and quality of life after the event [2,6].
Cerebral ischemia is a rare but significant complication of cervical disc herniation surgery, often caused by intraoperative carotid manipulation. Careful attention to the cervical vascular zone during surgery, with intermittent relaxations during retraction maneuvers, is essential to minimize this risk. Preoperative assessment of the carotid artery, particularly in at-risk patients, should be considered to prevent such complications.
The authors declare no competing interests.
Patient management and manuscript revision: Dahmane Elhairech and Mohamed Lmejatti. Data collection and manuscript drafting: Dahmane Elhairech. Both authors read and approved the final version of the manuscript.
Figure 1: magnetic resonance imaging scan displays two cervical disc herniations at C3-C4 and C4-C5, associated with disco-osteophytic spurs; arrows indicate the location of the disc herniations and thinning of the peri-medullary space
Figure 2: computed tomography scan in axial (A) and coronal (B) sections revealing a right temporo-parietal hypodensity, consistent with ischemic stroke in the Sylvian territory; arrows point to the area of ischemia
Figure 3: angioscan images in sagittal (A) and coronal (B) views showing an atherosclerotic plaque located in the right common carotid artery; arrows highlight the plaque in the respective sections
- Steinmetz MP, Benzel EC, editors. Benzel's Spine Surgery E-Book: Techniques, Complication Avoidance, and Management. Elsevier Health Sciences; 2016 Jun 29. Google Scholar
- Narain AS, Hijji FY, Khechen B, Haws BE, Louie PK, Bohl DD et al. Common medical complications following routine spinal surgery. In: Singh K, editor. Spinal essentials handbook. 1st ed. New York: Thieme; 2019. p. 232-43.
- Sugawara T. Neurologic complications in managing degenerative cervical myelopathy: pathogenesis, prevention, and management. Neurosurgery Clinics. 2018 Jan 1;29(1):129-37. PubMed | Google Scholar
- Vakharia K, Atwal GS, Levy EI. Management of Acute Ischemic Thrombosis. Neurosurg Clin N Am. 2018 Oct;29(4):595-604. PubMed | Google Scholar
- Dehkharghani S, Andre J. Imaging Approaches to Stroke and Neurovascular Disease. Neurosurgery. 2017 May 1;80(5):681-700. PubMed | Google Scholar
- Du YQ, Duan WR, Chen Z, Wu H, Jian FZ. Carotid Artery-Related Perioperative Stroke Following Anterior Cervical Spine Surgery: A Series of 3 Cases and Literature Review. J Stroke Cerebrovasc Dis. 2019 Feb;28(2):458-463. PubMed | Google Scholar