Cross-cultural adaptation and reliability of patient asthma knowledge questionnaire in the regional Indian language Marathi: a cross-sectional study
Vishakha Sitaram Nalage, Varoon Chandramohan Jaiswal, Deepika Sohan Burman, Ramya Anand Shetty, Akanksha Amarsingh Chauhan, Amruta Devendra Acharekar
Corresponding author: Vishakha Sitaram Nalage, Department of Cardiovascular and Respiratory Physiotherapy, Maharashtra Academy of Engineering and Educational Research┬┤s Physiotherapy College, Talegaon Dabhade, Pune, Maharashtra, India 
Received: 18 Oct 2022 - Accepted: 04 Jul 2024 - Published: 22 Jul 2024
Domain: Community health,Health education
Keywords: Bronchial asthma, cross-cultural adaptation, translation, disease-specific knowledge, patient education, Marathi language
©Vishakha Sitaram Nalage et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Vishakha Sitaram Nalage et al. Cross-cultural adaptation and reliability of patient asthma knowledge questionnaire in the regional Indian language Marathi: a cross-sectional study. Pan African Medical Journal. 2024;48:124. [doi: 10.11604/pamj.2024.48.124.37870]
Available online at: https://www.panafrican-med-journal.com//content/article/48/124/full
Research 
Cross-cultural adaptation and reliability of patient asthma knowledge questionnaire in the regional Indian language Marathi: a cross-sectional study
Cross-cultural adaptation and reliability of patient asthma knowledge questionnaire in the regional Indian language Marathi: a cross-sectional study
![]() Vishakha Sitaram Nalage1,&, Varoon Chandramohan Jaiswal1, Deepika Sohan Burman1, Ramya Anand Shetty1, Akanksha Amarsingh Chauhan1, Amruta Devendra Acharekar1
Vishakha Sitaram Nalage1,&, Varoon Chandramohan Jaiswal1, Deepika Sohan Burman1, Ramya Anand Shetty1, Akanksha Amarsingh Chauhan1, Amruta Devendra Acharekar1
&Corresponding author
Introduction: patient education is the cornerstone of the clinical management of bronchial asthma. The patient asthma knowledge questionnaire is a valid and reliable tool to assess the disease specific knowledge in the patients with bronchial asthma. To the best of our knowledge and literature search, there is no tool available in Marathi language to assess the knowledge of bronchial asthma in patients.
Methods: standard translation guidelines for cross-cultural adaptation were followed. Forward and backward translations were performed by the eligible translators (T1 and T2) as per the guidelines. Synthesis of the translated versions was performed by translators and recording observer (T12). Recommendations by the expert committee were done to develop a pre-final version. The pre-final version was then tested on 30 individuals with bronchial asthma. The reliability of the translated version was assessed by the internal consistency and intra-class correlation coefficient.
Results: thirty (30) bronchial asthma patients were recruited (with a mean age of 63SD±14.36, 16 male and 14 female) to test the pre-final version, and probing of each item was done to test the equivalence. It showed that the patient comprehended the intent behind each inquiry, and that was gauged on the Likert scale. A total of 102 adults (60.8% female and 39.2% male) with a mean age of 41±11 years were included in the study to examine test-retest reliability. Between the total scores obtained from the first and second applications of the questionnaire within a two-week period, there was no discernible variation. The internal consistency reliability (Cronbach´s alpha) was 0.79 and the Intra-class correlation coefficient was 1.000.
Conclusion: Marathi Version of the patient asthma knowledge questionnaire (PAKQ) is cross-culturally adapted and reliable; it will prove to be a beneficial tool to assess the disease-specific knowledge of bronchial asthma.
Bronchial asthma (BA) is a serious public health problem affecting individuals of all age groups and economic conditions. According to the World Health Organization (WHO) in 2016, asthma affected 235 million people globally, with 15 to 20 million of these individuals consisting of the Indian population [1-3]. Bronchial asthma management can be challenging and involves both the individual with BA and their family members. The patients need to learn specifics about their illness to control the disease effectively. It is well documented that insufficient disease-specific knowledge is one of the factors contributing to ineffective control in asthmatics [1-6]. Patient education programs have been found to be useful in increasing disease-specific knowledge and can be a contributing factor in the control of the disease. Developing an individually tailored educational program, and assessment of the disease-specific knowledge is of prime importance [1,5,7]. To successfully customize patient education in bronchial asthma, the disparities between disease-specific knowledge and self-management skills should be evaluated objectively. Self-reported questionnaires assessing patients´ knowledge can be a useful tool in narrowing these disparities, particularly if these tools are validated properly and in patients´ regional language. Specific patient education programs for BA patients use valid and reliable knowledge questionnaires to assess the patient´s knowledge and objectify the effect of the education program [1,5].
Valid and reliable questionnaires are available in various languages including English [1], French [3], Chinese [8], Spanish [9], Portuguese [10], and Turkish [11], but not Marathi. Marathi is the regional language in Maharashtra, India, but the best of our knowledge and literature search, currently there is no method to evaluate the knowledge of Marathi-speaking asthmatic patients. The Patient Asthma Knowledge Questionnaire is designed to explore aspects of asthma care and education program contents, such as asthma-specific knowledge, triggers, diagnostic tests, and asthma management among the patients. Patient asthma knowledge questionnaire was developed and validated by Beaurivage et al. in 2017 [1], is a questionnaire on asthma knowledge and self-management that is based on the core requirements outlined in the Global Initiative for Asthma (GINA) strategy report [1]. The measurement properties of the PAKQ were good in terms of content validity, face validity, criterion validity, construct validity consequences validity, reliability, and responsiveness [1]. It's crucial to note that this tool satisfies all of the validity criteria proposed by Pink et al. [12]. Hence we wanted to translate an equivalent Marathi version of the patient asthma knowledge questionnaire and check its reliability. The objective of the study is to translate an equivalent Marathi version of a patient asthma knowledge questionnaire and test its reliability. We hypothesised that the Marathi version of patient asthma knowledge questionnaire is well translated and reliable tool.
Study design: this cross-sectional study was approved by the institutional ethics committee. Permission from the author of the primary version of PAKQ was obtained to translate and adapt the questionnaire in the Marathi language.
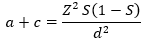
Participants and study size: sample size of 102 was calculated by using the formula:
Study settings and data sources: individuals diagnosed with bronchial asthma according to the GINA guidelines 2019, visiting the pulmonary outpatient department of Dr. Bhausaheb Sardesai Talegaon Rural Hospital were recruited in this study from July 2021 to December 2021.
Variable: the patient asthma knowledge questionnaire, is designed to explore aspects of asthma care and education program contents, such as asthma-specific knowledge, triggers, diagnostic tests, and asthma management among the patients. The patient asthma knowledge questionnaire was developed and validated by Beaurivage et al. in 2017 [1], is a questionnaire on asthma knowledge and self-management that is based on the core requirements outlined in the Global Initiative for Asthma (GINA) strategy report [1]. The measurement properties of the PAKQ were good in terms of content validity, face validity, criterion validity, construct validity consequences validity, reliability, and responsiveness [1]. It's crucial to note that this tool satisfies all of the validity criteria proposed by Pink et al. [12].
Study procedures: guidelines prescribed by Beaton et al. 2000 [13] to translate and adapt the self-report measures were followed to form the Marathi version of PAKQ. Six steps were completed to translate and adapt the PAKQ in Marathi Version;
Step 1; forward translation: the questionnaire was individually translated into Marathi by two bilingual translators with their mother tongue being Marathi (FT1 and FT2 Versions). Forward translator 1 was from medical background and forward translator 2 was from the community with no medical knowledge. Both translators submitted the report along with the translated copy provided to them. Local language, patient and grammatical contexts were considered by the translators during the process.
Step 2; synthesis of the FT1 and FT2: a common synthesized version T-12 was developed after reaching a consensus between the two forward translators and the recording observer. The English version of the questionnaire was taken as a reference during the entire process. A documented report of the synthesis process was maintained for further reference.
Step 3; backward translation: the synthesized version (T-12) was translated back into English by two back translators individually. Both the back translators were completely blind to the original concept and the questionnaire. Two back translated versions (BT1 & BT2) were submitted by the translators and synthesis was achieved (BT-12). BT-12 version was comparable to the original version of PAKQ. So, no changes were made by the authors in the T12 version.
Step 4; expert committee: pre-final version was prepared by the panel of experts consisting of a research methodologist, chest physician, language experts and all the translators. Expert committee recommendations were to include of the Indian brand name drugs and to keep the cognate words as it is in the questionnaire.
Step 5; test for the pre-final version: thirty (30) consecutive diagnosed cases of bronchial asthma visiting the pulmonary outpatient with a mean age of 63 (SD= 14.36, 16 male and 14 female) completed the questionnaire and were probed for the exact understanding of the items. All the participants were completed and probed under the supervision of same research assistant. All the participants completely understood the items of the pre-final version and no further changes were required.
Step 6; submission of the reports: all the reports and translated versions along with the final Marathi version of PAKQ was submitted to the original developers of the PAKQ and their approval was obtained. Test-retest reliability and internal consistency of PAKQ Marathi version. Informed consent was obtained from all the participants. All the patients filled in the questionnaire twice with a gap of 2 weeks. Test-retest reliability was calculated using the intraclass correlation coefficient (ICC) and Cronbach´s alpha coefficient was used to assess internal consistency.
Statistical methods: all the data processing and testing [8] was performed using IBM SPSS software 28.0 Version. Descriptive statistics were used to summarize the demographic characteristics and presented as n (%) or mean, standard deviation. Cronbach´s alpha was used to test internal consistency and test re-test reliability was tested using intra-class correlation.
Participants and descriptive data: a total of 102 adults (60.8% female and 39.2% male) with a mean age of 41±11 years were included in the study. According to the Global Initiative for Asthma (GINA) guidelines (2019), 60.78% of participants were considered with mild asthma, 39.21% with moderate asthma with an average duration of 11.6 years as shown in Table 1. For test-retest reliability, all the participants were recruited in order to complete the questionnaire twice. In the first observation, 102 (n=102) participants completed the questionnaire whereas in the second observation, only 90 (n=90) participants were able to complete it. Hence, we had 12 withdrawals since those participants were unable to make it to the hospital due to distance barriers.
Outcome data: in terms of internal consistency, the Marathi version of the PAKQ's Cronbach's alpha was estimated as 0.79, while the intraclass correlation coefficient was examined for test-retest reliability and is 1.000.
Main results: the Marathi version of the PAKQ has excellent intra-class reliability, as evidenced by the measurement of the intra-class correlation coefficient whereas the internal consistency was found to be acceptable by evaluating Cronbach´s alpha. This result revealed that all questions are consistent and measure the same concept [8].
The study aimed to translate, adapt, and evaluate the test-retest reliability and internal consistency of the PAKQ in Marathi language. Although there are number of questionnaries to study the bronchial asthma knowledge this is the first study intended to translate and adapt the questionnaire for Marathi-speaking individuals. The questionnaire was adapted as per the regional context according to the standard guidelines [13]. As per recommendations of the expert panel pharmacological drugs brand names in the original version were changed to the brand names of the Indian version eg: ( Budicort, AB Phylline, Sereflo, Montair, Asthalin, Foracort ) [14]. A complete and good understanding of all the items was seen during the testing of the prefinal version with 30 diagnosed cases of bronchial asthma. The test-retest reliability of the translated and adapted questionnaire was done using the interclass correlation coefficient. The interclass correlation coefficient measured for test-retest reliability was 1.000 with a 95% confidence interval as shown in Table 3 states the good reliability of the questionnaire. Whereas Cronbach´s alpha value calculated was 0.79 showing good internal consistency.
The original version of the PAKQ has already been tested for validity by the authors of the original version and published elsewhere [1]. The 54-item PAKQ Marathi version is, therefore, a valid and reliable tool with content that aligns with current international asthma guidelines and may therefore be of great help in regional clinical settings [1,3,8]. The questionnaire is easy to administer, appropriate, and intelligible to the target regional population to study the disease-specific knowledge. Marathi language has diverse dialects and a vast geographical regional population speaking the language so there can be few contextual differences while addressing the questionnaire to the entire region which can be addressed by closely monitoring the individual while completing the questionnaire. Also to the best of our knowledge, there is no Marathi asthma knowledge questionnaire previously verified our study did not compare the Marathi PAKQ with standard questionnaires to obtain concurrent validity [8].
The results of this study should be interpreted with caution. First, there may be a selection bias as the participants were recruited from only one tertiary health care center. Second, baseline educational qualification and socioeconomic criteria, which can affect the disease knowledge were not taken into consideration during the time of recruitment. Finally, it is important to validate and test the questionnaire with diverse participants with different cultures, demographics, and educational levels to confirm the generalizability of the tool. To summarize disease-specific knowledge is one important prognostic indicator of bronchial asthma. The lack of disease-specific self-report measures in the regional languages is a major barrier to the assessment of disease-specific knowledge of the individuals and implementation of the specific goal-based structured patient education programs. The questionnaire can be further utilized to study the disease specific knowledge and implementing the various bronchial asthma education programs, which is the integral part of the bronchial asthma management.
Marathi Version of the PAKQ is cross-culturally adapted and reliable; it will prove to be a multi-dimensional tool to assess the disease-specific knowledge of bronchial asthma amongst the Marathi speaking individuals.
What is known about this topic
- Patient education for asthma and its assessment using self-report measures is a well-established practice;
- Patient asthma knowledge questionnaire is already translated in English and Chinese languages and are both tested for their psychometric properties.
What this study adds
- This study has translated and adapted patient asthma knowledge questionnaire in regional Indian language Marathi;
- To the best of our knowledge, there is no instrument available to study the asthma specific knowledge in Marathi speaking individuals;
- This questionnaire will enhance the scope of asthma education in the clinical settings of Maharashtra India.
The authors declare no competing interest.
Vishakha Sitaram Nalage: conceptualization of the study and principal researcher; Varoon Chandramohan Jaiswal: conceptualization, formal analysis, investigations, methodology formation and study coordinator and manuscript writing; Deepika Sohan Burman: data collection and data curation visualization; Ramya Anand Shetty: methodology formation and writing; Akanksha Amarsingh Chauhan: data collection and data curation, validation and formal analysis; Amruta Devendra Acharekar: literature review. All the authors read and approved the final version of this manuscript.
We are grateful to Prof Louis-Philippe Boulet and Dr.Vanessa M. McDonald for the permission to translate and publishing of the PAKQ.
Table 1: distribution of age and gender of the participants
Table 2: mean, median and standard deviation of the participants
Table 3: intraclass correlation coefficient for test -retest reliability
- Beaurivage D, Boulet LP, Foster JM, Gibson PG, McDonald VM. Validation of the patient-completed asthma knowledge questionnaire (PAKQ). J Asthma. 2018 Feb;55(2):169-179. PubMed | Google Scholar
- AL-Jahdali H, Khan A, Shememeri A, Ahmad A, Al-Bader B, Al-Zahrani J et al. Factors associated with poor asthma control in the outpatient clinic setting. Ann Thorac Med . 2015 Apr-Jun;10(2):100-4. PubMed | Google Scholar
- Beaurivage D, Boulay ME, Frenette E, Boulet LP. Development and validation of patient´s knowledge measurement tools: The model of the Questionnaire de Connaissances sur l´Asthme destiné aux Patients Adultes (QCA-PA). Rev Mal Respir. 2016 May;33(5):350-64. PubMed | Google Scholar
- Schatz M, Sorkness CA, Li JT, Marcus P, Murray JJ, Nathan RA et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialistss. J Allergy Clin Immunol. 2006 Mar;117(3):549-56. PubMed | Google Scholar
- Borges MC, Ferraz É, Pontes SMR, Cetlin A de CVA, Caldeira RD, Silva CS da et al. Development and validation of an asthma knowledge questionnaire for use in Brazil. J Bras Pneumol. 2010 Jan-Feb;36(1):8-13. PubMed | Google Scholar
- Pinnock H, Parke HL, Panagioti M, Daines L, Pearce G, Epiphaniou E et al. Systematic meta-review of supported self-management for asthma: a healthcare perspective. BMC Med. 2017 Mar 17;15(1):64. PubMed | Google Scholar
- Gardner A, Kaplan B, Brown W, Krier-Morrow D, Rappaport S, Marcus L et al. National standards for asthma self-management education. Ann Allergy Asthma Immunol. 2015 Mar;114(3):178-186.e1 PubMed | Google Scholar
- Peng B, Sun L, Shang Y, Zhang Y, Gao X, Ye L et al. Translation and validation of the Chinese version of Patient-completed Asthma Knowledge Questionnaire and its implementation in patient education. J Thorac Dis. 2022 Apr;14(4):905-918. PubMed | Google Scholar
- López-Silvarrey Varela A, Pértega Díaz S, Rueda Esteban S, Korta Mur˙a J, Iglesias López B, Martínez-Gimeno A. Validation of a questionnaire in Spanish on asthma knowledge in teachers. Arch Bronconeumol. 2015 Mar;51(3):115-20. PubMed | Google Scholar
- Clérigo V, Cardoso B, Fernandes LS, Costa C, Garcia O, Tomaz E et al. Severe Asthma Questionnaire: translation to Portuguese and cross-cultural adaptation for its use in Portugal. Rev Port Imunoalergologia. 2019 Sep;27(3):233-42. Google Scholar
- Baygul A, Ozturk AB, Ozyigit LP, Keskin H, Karakaya G, Kalyoncu F et al. The Reliability and Validation of the Turkish Version of the Asthma Self-Management Knowledge Questionnaire. Turk Thorac J. 2017 Oct;18(4):125-130. PubMed | Google Scholar
- Pink J, Pink K, Elwyn G. Measuring patient knowledge of asthma: a systematic review of outcome measures. J Asthma. 2009 Dec;46(10):980-7. PubMed | Google Scholar
- Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976). 2000 Dec 15;25(24):3186-91. PubMed | Google Scholar
- Kritikos V, Krass I, Chan HS, Bosnic-Anticevich SZ. The validity and reliability of two asthma knowledge questionnaires. J Asthma. 2005 Nov;42(9):795-801. PubMed | Google Scholar











