Frequency and determinants of phytotherapy use in patients with type 2 diabetes in the Dschang Health District, Cameroon: a cross-sectional study
Michelle Carolle Dongmo Demanou, Sylvain Raoul Simeni Njonnou, André Arsène Bita Fouda, Eric Balti, Fernando Kemta Lekpa, Christian Ngongang Ouankou, Martine Claude Etoa Etoga, Cédric Fritz Gerald Eyenga Bangbang, Marie-Josiane Ntsama Essomba, Anne Ongmeb Boli, Fabrice Lekeufack, Dieudonné Désiré Michel Adiogo
Corresponding author: Sylvain Raoul Simeni Njonnou, Department of Internal Medicine and Specialties, Faculty of Medicine and Sciences Pharmaceutical of the University of Dschang, Dschang, Cameroon 
Received: 07 Sep 2023 - Accepted: 25 Feb 2024 - Published: 09 Apr 2024
Domain: Diabetes epidemiology,Diabetes care,Community health
Keywords: Phytotherapy consumption, type 2 diabetes, risk factors, Dschang, Cameroon
©Michelle Carolle Dongmo Demanou et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Michelle Carolle Dongmo Demanou et al. Frequency and determinants of phytotherapy use in patients with type 2 diabetes in the Dschang Health District, Cameroon: a cross-sectional study. Pan African Medical Journal. 2024;47:174. [doi: 10.11604/pamj.2024.47.174.41677]
Available online at: https://www.panafrican-med-journal.com//content/article/47/174/full
Research 
Frequency and determinants of phytotherapy use in patients with type 2 diabetes in the Dschang Health District, Cameroon: a cross-sectional study
Frequency and determinants of phytotherapy use in patients with type 2 diabetes in the Dschang Health District, Cameroon: a cross-sectional study
![]() Michelle Carolle Dongmo Demanou1,
Michelle Carolle Dongmo Demanou1, ![]() Sylvain Raoul Simeni Njonnou2,3,&,
Sylvain Raoul Simeni Njonnou2,3,&, ![]() André Arsène Bita Fouda1,
André Arsène Bita Fouda1, ![]() Eric Balti2,4,5,
Eric Balti2,4,5, ![]() Fernando Kemta Lekpa2,6,
Fernando Kemta Lekpa2,6, ![]() Christian Ngongang Ouankou2,7,
Christian Ngongang Ouankou2,7, ![]() Martine Claude Etoa Etoga5,8,
Martine Claude Etoa Etoga5,8, ![]() Cédric Fritz Gerald Eyenga Bangbang3,
Cédric Fritz Gerald Eyenga Bangbang3, ![]() Marie-Josiane Ntsama Essomba5,8,
Marie-Josiane Ntsama Essomba5,8, ![]() Anne Ongmeb Boli4,9, Fabrice Lekeufack10,
Anne Ongmeb Boli4,9, Fabrice Lekeufack10, ![]() Dieudonné Désiré Michel Adiogo11
Dieudonné Désiré Michel Adiogo11
&Corresponding author
Introduction: phytotherapy is widely used in Africa for the management of many diseases. Data on the use of phytotherapy in people with type 2 diabetes are scarce. We aimed to determine the frequency and factors associated with the consumption/use of phytotherapy products among patients with type 2 diabetes in the Dschang Health District.
Methods: we conducted a cross-sectional study from January to May 2022, including community-dwelling or hospitalized patients with type 2 diabetes who had lived in the Dschang Health District for at least one year. Informed consent was obtained from all patients. Data were collected using a pre-designed questionnaire. Variables collected included socio-demographic characteristics, diabetes knowledge and practices, and perceptions of care.
Results: we included 403 (249 women) patients with type 2 diabetes with a mean (SD) age of 63 (± 14.86) years). Among them, 240 (59.55%) used phytotherapy, either in combination with conventional treatment (168 (41.69%) participants) or not (72 (17.86%) participants), to treat diabetes. The most common reasons for using phytotherapy were easy accessibility and belief in its efficacy. Most patients used both treatments because they thought the combination was more effective. In univariable analysis, we observed a statistically significant association between level of education (p=0.003), socioeconomic level (p<0.001), place of residence (p=0.003), duration of diabetes (p=0.007), and use of phytotherapy. In multivariable analysis, only age between 51 and 60 years (OR: 0.50, 95% CI 0.298 - 0.8521; p=0.01) was associated with the use of phytotherapy.
Conclusion: people living with T2D in the Dschang Health District frequently use phytotherapy as an antidiabetic remedy, especially those aged between 51 and 60 years, those with low education level, low socioeconomic level and medium duration of diabetes. There is a need to evaluate its effectiveness in treating diabetes and its adverse effects.
Diabetes is a chronic metabolic disease characterized by elevated blood glucose (or blood sugar) levels, which over time leads to serious damage to the heart, blood vessels, eyes, kidneys, and nerves. It is recognized as a major cause of premature mortality and disability due to serious complications that can be both acute and chronic [1,2].
Worldwide, the prevalence of diabetes is estimated to be around 10% of the world's population, with 537 million people affected by diabetes in 2021, and the number of people affected is expected to increase in the coming years to 643 million in 2030 and 783 million in 2045. In addition, 6.7 million deaths are attributed to diabetes [2]. Despite advances in the management of type 2 diabetes mellitus (T2DM), treatment goals are often not achieved. Patients who are dissatisfied with the results of conventional medicine often turn to all or part of traditional medicine [3]. Traditional medicine is defined as "the total of knowledge, skills, and practices based on the theories, beliefs, and experiences of different cultures, whether explicable or not, which are used in the maintenance of health and the prevention, diagnosis, alleviation or treatment of physical or mental illness". One of the main components of traditional medicine is phytotherapy (or herbal medicine), which is the use of medicines derived from plants or herbs to treat or prevent health conditions [4]. A 2018 Canadian study found that 44% of patients used traditional medicines in combination with their conventional treatment [3]. Despite improvements in diabetes guidelines and care, patients in Western countries still use phytotherapy to treat diabetes [5-7].
In Africa, more than 24 million people will be living with diabetes in 2021, and approximately 416,000 deaths will be attributed to diabetes in 2021 [2]. Herbal medicine is used by 80% of the local population for primary health care and there is 1 healer per 500 people compared to 1 doctor per 40,000 people [4]. In rural areas, healers remain the healthcare providers for millions of people [4,8]. Studies carried out in 2015 and 2018 in Morocco and Algeria, respectively, found that factors associated with the use of herbal medicine by patients with T2DM were: low socioeconomic level, rural residence, and age at onset of diabetes [9,10]. In a study carried out in 2021 in an Ethiopian government hospital on 395 patients with T2DM, more than half of the patients used herbal medicine, in particular 58.5%. The factors favoring its use were: gender, place of residence, level of education, duration of the disease, and presence of complications related to diabetes [11].
Diabetes management is a real public health problem in Cameroon. The prevalence of diabetes is estimated at 5.5% in 2021 and could reach 8-40% in certain populations, such as groups of prisoners, as found in a 2020 study in Yaoundé Central Prison, or patients with stroke or chronic kidney disease [12-14]. In the West region of Cameroon, the use of herbal medicine for the treatment of many diseases, particularly diabetes, is part of an ancient tradition. Although there is little evidence of factors that favor its use in T2D patients, there is no data on the prevalence of phytotherapy consumption and its determinants. Based on this observation, we were motivated to conduct this study, the main objective of which was to determine the prevalence of phytotherapy consumption and identify the determinants, in order to improve the quality of health care for patients living with diabetes. in Cameroon.
Study design: a cross-sectional study was conducted on participants living with type 2 in the Dschang Health District (DHD) from January to May 2022.
Study setting and population: this study was carried out in the Dschang Health District. The latter follows the geographical contours of the Menoua subdivision in the Western Region of Cameroon. It covers a surface area of 1060 Km2 and is inhabited by around 240,000 people. Four of the six administrative precincts of Menoua are included in this health district (namely: Dschang; Fokoué; Nkong-ni; Fongo Tongo and the Fondonera group) (Dschang Health District) [15]. Many health facilities are present in this district, the main ones being Dschang Regional Hospital Annex (previously known as Dschang District Hospital), Saint Vincent de Paul Hospital, and Batsingla Hospital. These three health facilities each have an internal medicine department and a unit for monitoring people living with diabetes. The people living with diabetes are also organized in association at the level of the community.
Participants: the study population was patients living with type 2 diabetes followed in these three health facilities and/or living in the Dschang Health District. Patients with diabetes were defined as patients with a documented history of diabetes or meeting the American Diabetes Association 2022 criteria for diabetes who were considered diabetic, whether or not taking antidiabetic medication [16]. Participants were recruited at the Dschang District Hospital and in the community (homes, workplaces, and health centers). All participants were given clear information about the study and their participation. All participants with type 2 diabetes who had lived in the Dschang Health District for more than one year and who agreed to participate were included in the study. All pregnant participants with T2D and those who withdrew their consent during the study were excluded.
Variables: the collected variables included sociodemographic data, history of diabetes, treatment of diabetes, phytotherapy consumption, and its motivation. Phytotherapy (herbal medicine) was defined as a therapeutic method that uses plants or their extracts in the treatment of disease. Conventional medicine, on the other hand, was defined as the use of medicines purchased from a pharmacy. Drugs bought over the counter (street) were also considered as conventional medicine. Phytotherapy consumption was the outcome variable. Independent variables included the age, sex, educational level, religion, and the motivation for phytotherapy consumption. We considered possible confounders in our analysis.
Data resources and management
Data collection tool: data were collected using a pre-tested, standardized, anonymized questionnaire designed for this purpose. The information collected was then stored in a computer database. This structured questionnaire included all the above-listed variables.
Data collection: data were collected from the patient alone or, if necessary, in the presence of an interpreter with the patient's consent to facilitate communication. Patients were provided with an information leaflet explaining the aims of the study, and additional explanations were given if requested. Information was collected only after a positive response from the patient, who was given a consent form to sign. Information about the management of their disease was recorded. The study variables were socio-demographic data: age, sex, marital status, occupation, monthly income, region of origin, place of residence, religion, and level of education). Information on diabetes knowledge and practices was also collected: duration of diabetes, possession of a blood glucose meter, self-monitoring of blood glucose and type of treatment used. Data on perceptions of care (modern medicine, traditional medicine: exclusive use of one approach, combination of the two, therapeutic preference, elements of choice: cost; effectiveness; accessibility; cultural values) were also recorded. The type of treatment used and reason for using it were also registered.
Sample size: the sample size was calculated using Lorenz´s formula (Stat Calc of EPI Info Software). Using the national prevalence of 5.5% in Cameroon (according to IDF 2021 data), with an 80% power to detect significant associations or differences, and a 5% accepted margin of error. This gave us a minimum sample size of 80 patients using a margin of error of 5% (standard value of 0.05) [16].
Statistical analysis: the data collected on the survey sheets were processed on Excel® 2016 (Microsoft Corp., Washington, USA). This data was analyzed using Statistical Package for the Social Sciences® (SPSS) version 23.0 (Chicago, IL, USA). Qualitative variables were represented in frequencies and percentages by bar and sector tables and diagrams and quantitative variables were expressed by means and standard deviations. Chi-squared tests and logistic regressions allowed us to investigate the factors associated with the use of herbal medicine in DT2 patients. The significance threshold was defined as p less than 5% with a 95% confidence interval (CI).
Ethics approval and consent to participate: this work was approved by the Institutional Council of the Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon (Ethical Clearance 2959 CEI-Udo/02/2022/T from the Institutional Ethics Committee of the University of Douala for Human Health Research) and Obtaining Research Authorization from the Head of the DSD, the Director of the Dschang District Hospital (HDD). We conducted this study in strict compliance with the fundamental principles of scientific research in medicine. Patients were free to participate in the study without external constraints. We obtained an informed and signed consent form from each participant.
Sociodemographic analysis: we recruited 403 (249 women) T2D patients with a median age of 63 ± 14.86 years. Most of them were unemployed and had a monthly income lower than 50,000 FCFA (76.29 USD). Figure 1 presents the patient´s flow chart.
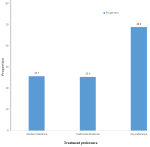
Frequency of phytotherapy products use: among our participants, 240 (59.55%) used phytotherapy, whether associated with conventional treatment (168 (41.69%) participants) or not (72 (17.86%) participants). The reasons for use declared by participants were: low cost (27.8%), ease of accessibility (36.1%), and belief in efficacy (36.1%). Most patients used both treatments because they thought the combination was more effective (69.1%). In addition, just over a quarter (25.7%) of participants preferred conventional treatment alone, while another quarter (24.4%) preferred herbal medicine alone, and almost half (48.9%) had no preference (Figure 2).
Bivariate analysis: in bivariable analysis, we observed an association between level of education (p=0.003), socioeconomic level (p <0.001), place of residence (p=0.003), duration of diabetes (p=0.007) and use of phytotherapy (Table 1).
Multivariate analysis: in multivariate analysis, only the age group between (51 and 60 years old) (OR: 0.50,95% CI 0.298 - 0.8521; p=0.01) was associated with the use of herbal medicine (Table 2). In addition, females were 1.5 times more likely to use phytotherapy and unemployed patients were 1.9 times more likely to use phytotherapy even though they were not associated with phytotherapy consumption. Similarly, having a monthly income of fewer than 25,000 FCFA (38.14 USD) increased the risk of using phytotherapy 2.6 times (Table 2).
The main objective of this study was to determine the prevalence and risk factors of phytotherapy use among patients with type 2 diabetes in a sub-Saharan Africa setting, the Dschang Health District in Cameroon. This study represents one of the few studies on the use of phytotherapy among T2D patients in Cameroon and showed frequently used phytotherapy as an antidiabetic remedy. Factors associated with its use were age between 51 and 60 years, low education level, low socioeconomic level, and medium duration of diabetes.
This cross-sectional study should be interpreted in light of some limitations. As we carried out this study in only one health district with urban and rural populations, findings can not be extrapolated to others. The other limitations were the size of the population (small), compared to other studies on the same topic, and the fact that much information relies on patient declarations. These could be inexact due to memory bias or lying. There is a great interest in the use, efficacy, and tolerability of phytotherapy in the management of T2D in Western and Asian countries. Recent studies in East and North African countries have shown a huge use of phytotherapy for the treatment of T2D with mixed results. To the best of our knowledge, there are no data on its prevalence and risk factors in Central Africa, particularly in Cameroon, when used to treat diabetes.
Of the participants included, the majority were female (61.8%) with a mean age of 63.77 ± 14.86 years. These findings corroborate a study by Alioune Camara et al. in 2014 and Simeni Njonnou et al. in 2020, where diabetes patients were predominantly female (61% and 66.2%, respectively) [17,18]. Doukani et al. also in Algeria in 2020, found that 58.75% of patients with diabetes were female [10]. An older population was also found by Youb et al. Selihi et al. and Hamza et al. [9,19,20]. This could be explained by the fact that insulin resistance increases with age and, in our context, women visit health facilities more often than men and their life expectancy is higher than that of men [14].
Almost a third (29.8%) of participants have never attended school while 44.4% had completed primary education. These results are similar to those found by Hamza et al. in 2011 in Algeria and Selihi et al. in Morocco where the majority of the participants of the patients were illiterate [9,20]. These findings are different from that of Doukani et al. in Algeria where there was no real difference among the study population concerning the educational level, as well as in a Canadian study [3,10]. This difference could be explained by the fact that the majority of the participants in our study came from rural areas and were of advanced age.
In this study, the percentage of T2D participants who used phytotherapy for the control or treatment of diabetes was 59.55%. This is similar to the results found in 2021 by Wahiba et al. (60%), and by Kasole et al. (67.2%) in Tanzania [21,22]. On the contrary, it is far superior to the results found in a Canadian study conducted by Grossman et al. in 2018 where the prevalence was 44% and also above 49% found in the literature in a study conducted by Hamza et al. in Algeria [3,20]. Our results could be explained by the fact that in our context, cultural values promote herbal medicine and access to care remains a real public health problem.
Participants aged between (60-80 years) used herbal the most (114 patients) while patients aged between (30-40 years) (4 patients) used less. This result is similar to the results found in the literature by Selihi et al. in Morocco where the majority of phytotherapy consumers (46.5%) were above the age of 60 [9]. However, these findings differ from the results found by Kasole et al. where T2D participants consuming phytotherapy were aged between (41 - 60 years) (59.8%) [22]. This could be explained by the fact that our study took into account patients living both in rural areas (who are mostly elderly) and in urban areas. Their attachment to traditional medicine could be explained by the fact that most patients in these age groups are much more attached to customs and traditions.
The prevalence of phytotherapy consumption among female T2D participants taking treatment was 82%. Similarly, the female gender had 1.5 times the risk of phytotherapy consumption compared to the male gender. Similar results were found in 2016 by Adouane et al. Doukani et al. and by Kasole et al. [10,22,23]. Hamdoun et al. and Errajraji et al. also found a significant association between female gender and phytotherapy consumption [24,25]. This result could be explained by the relatively high frequency of illiteracy of women in rural areas in our context, their vigilance for the balance of the disease, the ease of transmission of information between them, the lowest cost, the availability of traditional medicines, and women´s greater attachment to all that is traditional [26,27].
The majority of participants who used phytotherapy in our study were unemployed. Moreover, being unemployed increased 1.9 times the risk of using phytotherapy compared to the participants who were employed. In addition, in our study, there was a statistically significant association between occupation and phytotherapy consumption. The use of plants for the treatment of diabetes was also associated with low educational level, and low socioeconomic level. These results are similar to those found by Kasole et al. Hamdoun et al. Hamza et al. and Errajraji et al. where educational level and socioeconomic level were associated with the use of herbal medicine [20,22,24]. These studies corroborate the work by Selihi et al. on herbal medicine and degenerative complications of diabetes where the level of education, the socioeconomic level were significantly associated with the use of herbal medicine [9]. However, Doukani et al. found that the level of education had no significant influence on the use of phytotherapy to treat diabetes and the most represented socioeconomic level was the middle class [10]. These different elements favoring the use of plants, since in our context, care is generally the responsibility of patients or their families, thus limiting access to the conventional health system [27].
In this study, the majority of participants surveyed lived in rural areas (44.2%) with the majority of participants using phytotherapy. By the same, we had an association between residence location and the use of phytotherapy. This can be due to the fact they were very far away or did not have easy access to the medical centers supporting patients with diabetes. These results corroborate those found by Selihi et al. Hanae et al. and Doukari et al. where the majority of patients using herbal medicine lived in rural areas [9,10,28]. Some medical centers with general practitioners do not fully manage the disease due to insufficient technical support (lack of refrigerator for storing injectable antidiabetics and unavailability of all classes of oral antidiabetics) therefore use only available oral antidiabetics.
We found that participants whose duration in diabetes was between (5-10 years) used more herbal medicine (58.8%) compared to those whose duration was less than one year. In our study, the disease duration was associated with the use of herbal medicine. This is in line with the findings of Selihi et al. and Kasole et al. [9,22]. In addition, the use of medicinal plants can be explained by the fact that participants faced “relative inefficiency” of conventional treatment, as it fails to cure the disease and, if not well adapted, also fails to control glycemia and prevent chronic complications. [7].
Belief in efficacy, accessibility, and low cost were the main reasons driving phytotherapy consumption. This was similar to the results found in most studies in Africa although an influence of culture or tradition has been reported. [8-10,20,21,24]. Particular work should be done to bring treatment centers closer to patients and improve their technical platform.
Despite its limitations, this study which is to the best of our knowledge the first of its kind in Cameroon on T2D showed a huge consumption of phytotherapy in the Dschang Health District. Determinants of phytotherapy consumption in this study population included old age, residence in a rural area, and low income. The main reasons for consuming phytotherapy were the belief in efficacy, its accessibility, and its low cost. Important work should be done by stakeholders and medical staff to enhance patients´ education, and the technical level of treatment centers and bring them closer to patients. There is a need to evaluate its efficacy in treating diabetes and its adverse effects.
What is known about this topic
- Phytotherapy is widely used in sub-Saharan Africa for treating several diseases;
- Phytotherapy was used in many forms (barks, powder, decoctions) to treat diabetes.
What this study adds
- Almost 6 people over 10 with T2D are using phytotherapy;
- The main reasons for using it were: low cost (27.8%); accessibility (36.1%); and belief in efficacy (36.1%);
- In multivariate analysis, only the age group between (51 and 60 years old) was associated with the use of herbal medicine.
The authors declare no competing interests.
Design: Michelle Carolle Dongmo Demanou, André Arsène Bita Fouda, Dieudonné Désiré Michel Adiogo, Fabrice Lekeufack, and Sylvain Raoul Simeni Njonnou; data collection: Michelle Carolle Dongmo Demanou, Cédric Fritz Gerald Eyenga Bangbang, and Sylvain Raoul Simeni Njonnou; data analysis and interpretation: Michelle Carolle Dongmo Demanou, Cédric Fritz Gerald Eyenga Bangbang, Sylvain Raoul Simeni Njonnou, André Arsène Bita Fouda, Fernando Kemta Lekpa, and Dieudonné Désiré Michel Adiogo; manuscript writing: Sylvain Raoul Simeni Njonnou and Michelle Carolle Dongmo Demanou, Marie-Josiane Ntsama Essomba; manuscript revision: Eric Balti, Martine Claude Etoa Etoga, Christian Ngongang Ouankou, André Arsène Bita Fouda, Anne Ongmeb Boli, and Dieudonné Désiré Michel Adiogo. All the authors read and approved the final version of this manuscript.
We thank Professor Simeon Pierre Choukem for his help and his review of this article, the participants, and all the staff of the Diabetology Department of the Dschang Regional Hospital Annex and its Director Pr Michel Noubom.
Table 1: factors associated with the use of phytotherapy in univariate analysis among participants recruited in the Dschang Health District
Table 2: factors associated with the use of phytotherapy in multivariate analysis among participants recruited in the Dschang Health District
Figure 1: study population flowchart of participants recruited in the Dschang Health District
Figure 2: distribution of participants with type 2 diabetes recruited in the Dschang Health District by treatment preference
- Organisation mondiale de la Santé. Rapport mondial sur le diabète. Genève: Organisation mondiale de la Santé. 2016. Google Scholar
- Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022 Jan;183:109119. PubMed | Google Scholar
- Grossman LD, Roscoe R, Shack AR. Complementary and Alternative Medicine for Diabetes. Can J Diabetes. 2018;42 Suppl 1:S154-S161. PubMed | Google Scholar
- Organisation mondiale de la Santé. Stratégie de l´OMS pour la médecine traditionnelle pour 2014-2023. Genève: Organisation mondiale de la Santé. 2013. Google Scholar
- Barry JA. Living with type 2 diabetes mellitus in a modern Mexican city and opting for phytotherapy. Explore (NY). 2012 Jan-Feb;8(1):48-9. PubMed | Google Scholar
- Ruiz-Noa Y, Ibarra-Reynoso LDR, Ruiz-Padilla AJ, Alonso-Castro AJ, Ramírez-Morales MA, Zapata-Morales JR et al. Use of herbal medicine for diabetes mellitus in adults from the central-western region of Mexico. Prim Care Diabetes. 2021;15(6):1095-9. PubMed | Google Scholar
- Bell RA, Suerken CK, Grzywacz JG, Lang W, Quandt SA, Arcury TA. Complementary and alternative medicine use among adults with diabetes in the United States. Altern Ther Health Med. 2006;12(5):16-22. PubMed | Google Scholar
- Eddouks M, Ouahidi ML, Farid O, Moufid A, Khalidi A, Lemhadri A. L´utilisation des plantes médicinales dans le traitement du diabète au Maroc. Phytothérapie. 2007;5(4):194-203. Google Scholar
- Selihi Z, Berraho M, El Achhab Y, Nejjari C, Lyoussi B. Phytothérapie et complications dégénératives du diabète de type 2: quelle relation. Médecine Mal Métaboliques. 2015;9(8):792-7. Google Scholar
- Doukani C, Soltani R. Enquête éthnobotanique des plantes médicinales et alimentaires antidiabétiques à Tébessa. 2020. Google Scholar
- Kifle ZD, Bayleyegn B, Yimer Tadesse T, Woldeyohanins AE. Prevalence and associated factors of herbal medicine use among adult diabetes mellitus patients at government hospital, Ethiopia: An institutional-based cross-sectional study. Metabol Open. 2021 Aug 26;11:100120. PubMed | Google Scholar
- Patrice HM, Pascal KA, François KF, Hilaire D, Solange DM, Gloria AE et al. Markers and risk factors for chronic kidney disease in sub-Saharan Africans: baseline levels and 12-month trajectories in newly referred patients in Cameroon. BMC Nephrol. 2020;21(1):101. PubMed | Google Scholar
- Massi DG, Doumbe J, Patouokoumche RN, Ayeah CM, Kenmegne C, Mapoure YN. Outcome between Diabetic versus Non-Diabetic Acute Stroke in a Black African Population: A Cohort Study. WJNS. 2021;11(03):231-45. Google Scholar
- Simeni Njonnou SR, Boombhi J, Etoa Etoga MC, Tiodoung Timnou A, Jingi AM, Nkem Efon K et al. Prevalence of Diabetes and Associated Risk Factors among a Group of Prisoners in the Yaoundé Central Prison. J Diabetes Res. 2020 Jan 24;2020:5016327. PubMed | Google Scholar
- Ministère de la Santé Publique du Cameroun- Carte sanitaire. Regions de Sante du Cameroun. Accessed 7th September 2023.
- Nzechieu Evenge CN, Zeuko'o Menkem E, Ngounou E, Watching D, Nembu EN, Luma WS et al. Prevalence of hepatitis B and associated factors in the Buea Regional Hospital, Cameroon. Heliyon. 2023 Jul 4;9(7):e17745. PubMed | Google Scholar
- Camara A. Facteurs associés au mauvais contrôle glycémique dans une population de diabétiques de type 2 de l´Afrique Sub-saharienne. 2014. Google Scholar
- Simeni Njonnou SR, Tiodoung Timnou A, Etoa Etoga MC, Musa Jingi A, Boombhi J, Nganou-Ngnindjo CN et al. Impact of rest on office blood pressure in patients with hypertension and diabetes at the national obesity centre of Yaounde: a cross-sectional study in Sub-Saharan Africa. J Xiangya Med. 2020;5(2):1-8. Google Scholar
- Youb I, Karamane S. Profil lipidique chez les diabétiques type 2 et contribution à l´étude phytochimique de quelques plantes médicinales antidiabétiques. 2017.
- Hamza N, Agli AN, Moore N. Effets préventif et curatif de trois plantes médicinales utilisées dans la Wilaya de Constantine pour le traitement du diabète de type 2 expérimental induit par le régime « high fat » chez la souris C57BL/6J. 2011:1-107. Google Scholar
- Wahiba K. Survey on the use of phytotherapy in a officine in the region grande Casablanaca. Mohammed V-Rabat University, Faculty of Medicine and Pharmacy. 2020.
- Kasole R, Martin HD, Kimiywe J. Traditional Medicine and Its Role in the Management of Diabetes Mellitus: "Patients' and Herbalists' Perspectives". Evid Based Complement Alternat Med. 2019 Jul 4;2019:2835691. PubMed | Google Scholar
- Adouane S. Etude ethnobotanique des plantes médicinales dans la région méridionale des Aurès. 2016. Google Scholar
- Hamdoun W. Enquâte sur l´usage de la phytothérapie au sein d´une officine dans la région du grand casablanaca. 2021. Google Scholar
- Errajraji A, Ouhdouch F, El-Anssari N. Usage des plantes médicinales dans le traitement du diabète de type 2 au Maroc: Use of medicinal plants for type 2 diabetes treatment, in Morocco. Médecine Mal Métaboliques. 2010;4(3):301-4. Google Scholar
- Mudonhi N, Nunu WN. Traditional Medicine Utilisation Among Pregnant Women in Sub-saharan African Countries: A Systematic Review of Literature. Inquiry. 2022;59:00469580221088618. PubMed | Google Scholar
- Azevedo MJ, Azevedo MJ. The State of Health System(s) in Africa: Challenges and Opportunities. Historical Perspectives on the State of Health and Health Systems in Africa, Volume II: the modern era. 2017;1-73. Google Scholar
- Hanae B. Les plantes médicinales et diabète de type 2(A propos de 199 cas). 2012:1-106. Google Scholar
Search
This article authors
On Pubmed
- Michelle Carolle Dongmo Demanou
- Sylvain Raoul Simeni Njonnou
- André Arsène Bita Fouda
- Eric Balti
- Fernando Kemta Lekpa
- Christian Ngongang Ouankou
- Martine Claude Etoa Etoga
- Cédric Fritz Gerald Eyenga Bangbang
- Marie-Josiane Ntsama Essomba
- Anne Ongmeb Boli
- Fabrice Lekeufack
- Dieudonné Désiré Michel Adiogo
On Google Scholar
- Michelle Carolle Dongmo Demanou
- Sylvain Raoul Simeni Njonnou
- André Arsène Bita Fouda
- Eric Balti
- Fernando Kemta Lekpa
- Christian Ngongang Ouankou
- Martine Claude Etoa Etoga
- Cédric Fritz Gerald Eyenga Bangbang
- Marie-Josiane Ntsama Essomba
- Anne Ongmeb Boli
- Fabrice Lekeufack
- Dieudonné Désiré Michel Adiogo