Assessment of knowledge and acceptability of HIV self-testing among students of selected universities in southwest Nigeria: an online cross-sectional study
Abdulhammed Opeyemi Babatunde, Progress Agboola, Yusuf Babatunde, Esther Bosede Ilesanmi, Habibllah Ayodele, Oliver Chukwujekwu Ezechi
Corresponding author: Abdulhammed Opeyemi Babatunde, Medicine and Surgery, Faculty of Clinical Sciences, College of Medicine, University of Ibadan, Ibadan, Nigeria 
Received: 24 Sep 2021 - Accepted: 20 Mar 2022 - Published: 24 Oct 2022
Domain: HIV epidemiology,Global health,Public health
Keywords: Nigeria, students, university, HIV/AIDs
©Abdulhammed Opeyemi Babatunde et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Abdulhammed Opeyemi Babatunde et al. Assessment of knowledge and acceptability of HIV self-testing among students of selected universities in southwest Nigeria: an online cross-sectional study. Pan African Medical Journal. 2022;43:94. [doi: 10.11604/pamj.2022.43.94.31741]
Available online at: https://www.panafrican-med-journal.com//content/article/43/94/full
Research 
Assessment of knowledge and acceptability of HIV self-testing among students of selected universities in southwest Nigeria: an online cross-sectional study
Assessment of knowledge and acceptability of HIV self-testing among students of selected universities in southwest Nigeria: an online cross-sectional study
![]() Abdulhammed Opeyemi Babatunde1,2,&, Progress Agboola3, Yusuf Babatunde2,4, Esther Bosede Ilesanmi5, Habibllah Ayodele6,
Abdulhammed Opeyemi Babatunde1,2,&, Progress Agboola3, Yusuf Babatunde2,4, Esther Bosede Ilesanmi5, Habibllah Ayodele6, ![]() Oliver Chukwujekwu Ezechi7,8,9
Oliver Chukwujekwu Ezechi7,8,9
&Corresponding author
Introduction: in Nigeria, it was estimated that 1.9 million people were living with HIV of which 130,000 people were newly infected with HIV. HIV self-testing would potentially increase access to HIV testing for people to know their status, get diagnosed, and initiate treatment as soon as possible. Our study aims to assess the knowledge of HIV Self-Testing (HIVST) and the acceptability of this youth-friendly approach among students in southwest Nigeria online.
Methods: a cross-sectional study was conducted among bona fide undergraduate students (2019/2020 session) of two popular tertiary institutions in southwest Nigeria. An online standardized self-administered questionnaire was administered using Google Forms. Microsoft Excel and IBM SPSS statistics were used for tabulation and statistical data analysis. The Chi-Square test was conducted using a P value of 0.05 to determine the level of significance.
Results: of the 155 students that participated in the study, 82 (52.9%) were male. Most of the respondents (65.2%) were studying medicine and other health-related courses. The mean knowledge of HIVST among respondents was slightly above average. Respondents studying medical and other health-related courses showed a slightly better level of knowledge than others although not statistically significant (P = 0.222). 76.1% of respondents had never used the HIVST option before and 62.6% are willing to use it sometimes in the future.
Conclusion: to achieve the UNAIDS 95-95-95 fast-track targets in Nigeria by 2030, there is a need to promote sexual and reproductive health education and increase awareness and accessibility of HIVST to youths.
It was estimated in 2017 that 36.9 million (31.1-43.9 million) persons were living with HIV and 21.7 million (19.1-22.6 million) were getting access to antiretroviral therapy (ART) worldwide [1]. The Joint United Nations Programme on HIV/AIDS (UNAIDS) has introduced a formidable global 95-95-95 target to be achieved by 2030. The goal is to reach 95% of adults who know their HIV status, 95% of those who are HIV positive are accessing ART services, and 95% of those enrolled in ART have viral suppression by 2030. However, the usual HIV testing services (HTS) are not effective and adequate to attain universal access to HIV prevention, treatment, and management, especially for those that have not been tested, those at higher risk of contracting HIV, and marginalized populations [1].
In sub-Saharan Africa, only 40% of people living with HIV (PLHIV) know their HIV status even with the availability of HIV testing service centres across the regions [1]. Nigeria has the second-highest number of PLHIV who are unaware of their status. In Nigeria in 2018, it was estimated that 1.9 million people were living with HIV of which 130,000 people were newly infected with HIV and 53,000 people died from an AIDS-related illness [2]. Out of the confirmed population, 67% of people living with HIV knew their status, 53% of people living with HIV were on treatment and 42% of people living with HIV were virally suppressed [2].
To meet UNAIDS ambitious goal, there is a need for increased HIV testing and ensuring that no one is left behind. The concept of HIV self-testing is to make HIV testing more convenient and ensure privacy through a youth-friendly approach. There have been concerns about stigma and confidentiality which limits the uptake of HIV testing among young adults [3]. Also, for a key population of groups including men who have sex with men (MSM), female sex workers, and injecting drug users, the uptake of HIV testing services is often reduced due to several factors such as stigma and discrimination, criminalization, and fear of having trouble with law enforcement authorities [3].
HIV self-testing can increase the number of people living with HIV who have access to testing, know their status, are diagnosed, and initiate treatment as soon as possible [4]. To overcome barriers to HIV testing uptake, the World Health Organization (WHO) developed HIV guidelines recommending HIV self-testing (HIVST) be offered in addition to existing facility-testing modalities (2016) [5]. Oral HIVST involves the person obtaining an oral sample by swiping the gums with the appropriate test swab, doing the test, and analysing the test's result privately. It is said to be a screening test and does not indicate a definitive diagnosis; thus, it requires confirmative testing [3].
The HIVST policy landscape is changing rapidly. Following the release of the WHO guidelines in 2016, many countries including Nigeria have been quick to take up HIVST national policies and have already begun to implement various approaches [6]. In considering the need to adopt these innovative approaches to ensure more people access HIV diagnosis and get treatment, HIVST remains an effective new way to reach more people than what is currently available through normal facility visits and testing. Some quantitative studies have been conducted in other African countries to access the acceptability and feasibility of HIVST among young people in Africa, however, none has been carried out in Nigeria [7-10]. Although a recent study evaluated the preference for HIVST among young Nigerians using a qualitative approach [11].
Our study aims to assess the knowledge of HIV self-testing and the acceptability of this youth-friendly approach among undergraduate students in southwest Nigeria. This study also assesses the relationship between the knowledge of HIV self-testing and the socio-demographic characteristics of students.
Study design: this study employed a cross-sectional study design among current undergraduate students of two popular tertiary institutions in southwest Nigeria - the University of Ibadan, Ibadan, Nigeria, and the Ladoke Akintola University of Technology, Ogbomoso, Nigeria
Study setting: Nigeria is the most populous country in Africa, with an estimated population of 200 million and about 1.8 million people living with HIV. South West Nigeria is one of the geopolitical zones of Nigeria consisting of six States and is mainly populated by the Yoruba tribe. The University of Ibadan and the Ladoke Akintola University of Technology are two major universities in this region with about 30,000 students each.
Sample size estimation: the convenient sampling technique was adopted in the study. No prior sample size was calculated. The survey was online-based and required the voluntary participation of eligible students with access to the internet.
Study instrument and administration: the study questionnaire was developed from previous studies on knowledge and willingness to use HIVST and modified by the researchers to fit the objectives of this study [12,13]. Next, a pre-test was conducted by members of the research team to examine for readability, comprehensibility and grammatical error. The final questionnaire was validated by Sexual and Reproductive Health experts comprising sections on socio-demographic characteristics, awareness, and knowledge of HIVST, and acceptability of HIVST. The final questionnaire was then used to develop the online survey using Google form and a link to the e-survey was shared.
Study participants: study participants included all current undergraduate students of the University of Ibadan, Ibadan, Nigeria, and the Ladoke Akintola University of Technology, Ogbomoso, Nigeria with access to the internet. A convenient sampling technique was used. A standardized self-administered questionnaire was designed using google forms and the link to the questionnaire was sent to students and student groups of both universities via WhatsApp and Facebook. The voluntary response and snowball sampling techniques were adopted. Eligible respondents were encouraged to send the link to other prospective respondents on their WhatsApp contact list and share it on other online platforms. The standardized questionnaire conformed to the Helsinki Declaration, the purpose of the study was explained to each participant and informed consent was provided on the first page of the questionnaire where a participant could willingly choose whether or not to participate in the study. The online questionnaire was employed as a result of the closure of institutions as an intervention to mitigate the spread of the COVID-19 pandemic in the country. Besides, the study population is students who are most active on the internet, have access to mobile phones, and also understand the English language. The study was carried out over one month in September 2020. A total of 155 students were enrolled.
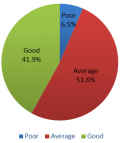
Study variables and data sources: the online questionnaire used in this study was drafted in English Language and piloted among 10 members of the research team for validation before sharing online. It comprised of three sections which included: socio-demographic characteristics, the knowledge and awareness of HIV-Self-Testing, and acceptability of HIV-Self-Testing. The socio-demographic variables included gender, age, marital status, level of study, and type of student (whether medical or health-related student or not). The level of knowledge and awareness of HIV-Self-Testing was determined through a five-point Likert-type scale about whether the respondents ‘strongly disagree’, ‘disagree’, ‘neutral’, ‘agree’, or ‘strongly agree’ and consisted of twelve (12) items, eight of which tested for knowledge while others tested for awareness. Knowledge items were given a score of 1 for ‘strongly agree’ or ‘agree’ while ‘neutral’, ‘disagree’ or ‘strongly disagree’ was given a score of 0 for a positively phrased question and vice versa for negatively phrased questions. Total knowledge score (range = 0 to 8) were arbitrarily categorized into 0-2 = poor, 3-5 = average, and 6-8 = good. Level of acceptability of HIV Self-Testing comprised of eight (8) items answered as either ‘Yes’, ‘No’ or ‘I don't know’.
Bias: potential sources of bias for this study were from the method of data collection which was online. This was controlled for, in the study design by including the name of schools and simple questions about the school which is expected to be known by all students of the respective schools. Also, the links were shared through student platforms and a study was conducted for a short time to reduce spam.
Quantitative variables and statistical methods: the data collected online was saved to Microsoft Excel for cleaning and re-coding and then exported to IBM SPSS Statistics version 20 for tabulation and statistical data analysis. Descriptive analysis for frequency and inferential statistics with the Chi-Square test was conducted. A P value of 0.05 at a 95% confidence interval was used to determine the level of significance of the variables.
Ethical consideration: the study was conducted during the COVID-19 lockdown and no formal ethical approval was collected from the institution's ethical review body. However, we adhered strictly to all the ethical issues involved in conducting studies involving human participants such as informed consent which was obtained electronically and clearly stated participants' rights to withdraw anytime from the study. Besides, we ensured confidentiality and anonymity by not requesting any personal or identifiable codes on the online survey.
Participants: the total number of responses recorded was 156 while only the data from 155 respondents who consented to participate in the study was included in the analysis.
Descriptive data: of the 155 students that participated in the study, 82 (52.9%) were male. The majority (58.1%) were within the age range of 21-25 years old. The majority (64.5%) of the participants were students from the University of Ibadan. Most of the respondents (65.2%) were studying medicine and other health-related courses. Table 1 shows the socio-demographic characteristics of respondents.
Outcome data: about 6.5% of the respondents had poor knowledge of HIVST (Figure 1). The mean knowledge of HIVST among respondents was slightly above average (mean = 5.1, median = 5, SD = 1.4). Most of the respondents gave a wrong answer to the question testing their understanding of the principle guiding HIVST kit about the reactivity of antibodies with reagents. Only 36% understood that HIVST kits were not reusable. 94.2% of respondents were aware of the need for a confirmatory diagnostic test in the hospital if tested positive with an HIVST kit (Table 2). About seventy-six percent (76.1%) of respondents have never used the HIVST option before and 62.6% are willing to use it sometimes in the future. Most respondents prefer HIV counselling and testing (HCT) to HIVST (52.3% and 32.3% respectively). However, there is average general acceptability (56.9%) of HIVST (Table 3). There was no statistically significant difference between the level of knowledge and any of the socio-demographic characteristics although respondents studying medical and other health-related courses showed a slightly better level of knowledge than others (P = 0.222).
This study investigated the knowledge and acceptability of HIV self-testing (HIVST) amongst students of selected universities in southern Nigeria. Majority of the respondents were youths and single. From our results, there was no considerable difference between the level of knowledge and any of the socio-demographic characteristics. However, respondents studying medical and other health-related courses showed a slightly better level of knowledge than others. The findings of this study revealed average knowledge (51.6%) and high acceptability (62.6%) of HIVST among students of selected universities in southern Nigeria. The results from our study had similar proportions in terms of knowledge of HIVST in other African institutions [14,15]. Although, the level of acceptability was higher in other parts of Africa (70% - 87.1%) [14-21], and Canada (81%) [22]. The lower acceptance among our respondents when compared to other studies across Africa and Canada could be because of variations in prevalence, the intensity of HIV interventions, and cultural differences as well as incentives [23-26].
Despite the high level of acceptability of HIVST, most students had concerns and preferred HIV counselling and testing (HCT) to HIVST (52.3% and 32.3% respectively). The possible reasons were not investigated in this study. These concerns were in sync with a study conducted in Tanzania to determine the level of knowledge, acceptability, and willingness to use oral fluid HIV self-testing among medical students. Findings from the study revealed that lack of pre and post-test counselling after self-testing was a key concern among the respondents [27]. These concerns also concur with findings from different settings highlighting the importance of HCT and HIVST [28-34].
In addition, 65.2% of the respondents were ready to pay for the HIVST kit. A previous study conducted has reported that the cost of purchasing a self-test kit is one of the major barriers that hinder willingness to use and conduct HIVST [28,29,33,35,36]. Our study was in sync with many other studies assessing willingness to HIVST in other different settings [37-39] but contrary to the findings from Hlongwa et al. among medical students in Tanzania [27]. The reason for the contrary result could be because of the economical differences between Nigeria and Tanzania [27]. This comparison is really important in addressing the issue of the cost of acquiring these HIVST kits, particularly among young people in low-income countries, to increase the uptake of HIVST. According to Nyblade et al., in sub-Saharan Africa, the cost to purchase HIVST kits will likely compete with daily necessities such as food due to high levels of poverty when compared to high-income countries [40].
Global evidence has suggested that HIVST has the potential to overcome the existing barriers with existing HIV testing interventions [41]. Barriers such as fear of stigma and discrimination, lack of privacy and confidentiality, and hard-to-reach key populations affect already existing HIV testing services [37-41]. It is therefore key to develop interventions that ensure proper awareness of HIVST to all populations and ensure HIVST and its concept are incorporated into the pre-service curriculum for medical and health-related courses. There is a high potential for HIVST to reach key populations at high risk of HIV/AIDS and this means specific measures and innovations like the cost of the self-kits, delivering the kits to people in the comfort of their homes and much more has to be addressed to ensure HIVST is acceptable by all.
Limitations: the study aimed at assessing the knowledge and acceptability of HIVST among students of selected Universities. However, some limitations and sources of biases were identified. Due to the sampling method used in data collection, most of the respondents were students from Health Sciences who are expected to have basic knowledge of HIVST. Another limitation of our study is the sample size but it covers a key insight into the knowledge and acceptability of HIVST. Also, based on the convenient sampling technique used and the method of data collection which is online, our study could have omitted some students with limited or no access to the internet hence, the results may not represent the general population.
Our study indicates average knowledge and moderate acceptability of HIVST among the selected students without any significant association with socio-demographic characteristics. However, there is a need to promote awareness about HIVST among youths in Nigeria to achieve the UNAIDS 95-95-95 fast-track targets by 2030 [41].
What is known about this topic
- More than half of people living with HIV in Africa do not know their status;
- HIV prevalence is high in Nigeria, especially among the youths.
What this study adds
- University students have an average level of knowledge about HIV Self-Testing;
- HIV Self-Testing has the potential to be acceptable by University students;
- There is no significant association between socio-demographic characteristics and the level of knowledge about HIV Self-Testing among participants.
The authors declare no competing interests.
Abdulhammed Opeyemi Babatunde conceptualized and designed the study; Abdulhammed Opeyemi Babatunde, Progress Agboola, Yusuf Babatunde, Esther Bosede Ilesanmi and Habibllah Ayodele wrote the first draft of the manuscript; Oliver Chukwujekwu Ezechi reviewed the final manuscript. All authors read and approved the final version of the manuscript.
Table 1: socio-demographic characteristics of respondents
Table 2: selected items measuring knowledge on HIV self-testing (HIVST)
Table 3: selected items on the level of acceptability of HIV self-testing
Figure 1: level of Knowledge of HIVST among respondents
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Global AIDS Update 2018 Miles To Go: Closing Gaps Breaking Barriers Righting Injustices. Unaids [Internet].
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Nigeria. 2020.
- Tun W, Vu L, Dirisu O, Sekoni A, Shoyemi E, Njab J et al. Uptake of HIV self-testing and linkage to treatment among men who have sex with men (MSM) in Nigeria: A pilot programme using key opinion leaders to reach MSM. J Int AIDS Soc. 2018;21(2016):e25124. PubMed | Google Scholar
- World Health Organization. HIV Self-Testing. 2014;(2):12-31.
- World Health Organization. Guidelines on HIV self-testing and partner notification: supplement to consolidated guidelines on HIV testing services. December 2016. Google Scholar
- UNITAID Innovation in Global Health. HIV rapid diagnostics for self-testing: 3rd edition. 2017.
- Thirumurthy H, Masters SH, Mavedzenge SN, Maman S, Omanga E, Agot K. Promoting male partner HIV testing and safer sexual decision making through secondary distribution of self-tests by HIV-negative female sex workers and women receiving antenatal and post-partum care in Kenya: a cohort study. Lancet HIV. 2016;3(6):e266-74. PubMed | Google Scholar
- Choko AT, MacPherson P, Webb EL, Willey BA, Feasy H, Sambakunsi R et al. Uptake, accuracy, safety, and linkage into care over two years of promoting annual self-testing for HIV in Blantyre, Malawi: a community-based prospective study. PLoS Med. 2015;12(9):e1001873. PubMed | Google Scholar
- Hatzold K, Gudukeya S, Mutseta MN, Chilongosi R, Nalubamba M, Nkhoma C et al. HIV self-testing: breaking the barriers to uptake of testing among men and adolescents in sub-Saharan Africa, experiences from STAR demonstration projects in Malawi, Zambia and Zimbabwe. J Int AIDS Soc. 2019;22(S1):e25244. PubMed | Google Scholar
- Indravudh PP, Sibanda EL, d'Elbee M, Kumwenda MK, Ringwald B, Maringwa G et al. ‘I will choose when to test, where I want to test´: investigating young people´s preferences for HIV self-testing in Malawi and Zimbabwe. AIDS. 2017;31(Suppl 3):S203-12. PubMed | Google Scholar
- Obiezu-Umeh C, Gbajabiamila T, Ezechi O, Nwaozuru U, Ong JJ, Idigbe I et al. Young people´s preferences for HIV self-testing services in Nigeria: a qualitative analysis. BMC Public Health 2021;21(67). Google Scholar
- Vara PA, Buhulula LS, Mohammed FA, Njau B. Level of knowledge, acceptability, and willingness to use oral fluid HIV self-testing among medical students in Kilimanjaro region, Tanzania: a descriptive cross-sectional study. AIDS Res Ther. 2020 Sep 9;17(1):56. PubMed | Google Scholar
- Johnson C, Neuman M, MacPherson P, Choko A, Quinn C, Wong VJ et al. Use and awareness of and willingness to self-test for HIV: an analysis of cross-sectional population-based surveys in Malawi and Zimbabwe. BMC Public Health. 2020 May 25;20(1):779. PubMed | Google Scholar
- Mokgatle MM, Madiba S. High acceptability of HIV self-testing among technical vocational education and training college students in Gauteng and North West Province: what are the implications for the scale up in South Africa? PLoS One. 2017;12:e0169765. PubMed | Google Scholar
- Izizag BB, Situakibanza H, Mbutiwi T, Ingwe R, Kiazayawoko F, Nkodila A et al. Factors associated with acceptability of HIV self-testing (HIVST) among university students in a Peri-Urban area of the Democratic Republic of Congo (DRC). Pan Afr Med J. 2018;31:248. PubMed | Google Scholar
- Zanolini A, Chipungu J, Vinikoor MJ, Bosomprah S, Mafwenko M, Holmes CB et al. HIV self-testing in Lusaka Province, Zambia: acceptability, comprehension of testing instructions, and individual preferences for self-test kit distribution in a population-based sample of adolescents and adults. AIDS Res Hum Retroviruses. 2018;34(3):254-260. PubMed | Google Scholar
- Kalibala S, Tun W, Cherutich P. Factors associated with acceptability of HIV self-testing among health care workers in Kenya. AIDS Behav. 2014;18:S405-S414. PubMed | Google Scholar
- Kebede B, Abate T, Mekonnen D. HIV self-testing practices among Health Care Workers: feasibility and options for accelerating HIV testing services in Ethiopia. Pan Afr Med J. 2013;15:50. PubMed | Google Scholar
- Kumwenda M, Munthali A, Phiri M, Mwale D, Gutteberg T, MacPherson E et al. Factors shaping initial decision-making to self-test amongst cohabiting couples in urban Blantyre, Malawi. AIDS Behav. 2014;18 Suppl 4(Suppl 4):S396-404. PubMed | Google Scholar
- Tonen-Wolyec S, Mbopi-Keou F, Batina-Agasa S, Kalla GCM, Noubom M, Bouassa RSM et al. Acceptability of HIV self-testing in African students: a cross-sectional survey in the Democratic Republic of Congo. Pan Afr Med J. 2019;33:83. PubMed | Google Scholar
- Iliyasu Z, Kassim RB, Iliyasu BZ, Amole TG, Nass NS, Marryshow SE et al. Acceptability and correlates of HIV self-testing among university students in northern Nigeria. Int J STD AIDS. 2020;31(9):820-831. PubMed | Google Scholar
- Brown B, Folayan MO, Imosili A, Durueke F, Amuamuziam A. HIV self-testing in Nigeria: public opinions and perspectives. Glob Public Health. 2015;10(3):354-365. PubMed | Google Scholar
- Carballo-Diéguez A, Frasca T, Balan I, Ibitoye M, Dolezal C. Use of a rapid HIV home test prevents HIV exposure in a high risk sample of men who have sex with men. AIDS Behav. 2012;16(7):1753-1760. PubMed | Google Scholar
- Gaydos CA, Hsieh YH, Harvey L, Burah A, Won H, Jett-Goheen M et al. Will patients “opt in” to perform their own rapid HIV test in the emergency departments? Ann Emerg Med. 2011 Jul;58(1 Suppl 1):S74–S78. PubMed | Google Scholar
- Spielberg F, Critchlow C, Vittinghoff E, Coletti AS, Sheppard H, Mayer KH et al. Home collection for frequent HIV testing: acceptability of oral fluids, dried blood spots and telephone results. HIV Early Detection Study Group. AIDS. 2000;14(12):1819-1828. PubMed | Google Scholar
- Osmond DH, Catania J, Pollack L, Canchola J, Jaffe D, MacKellar D et al. Obtaining HIV test results with a home collection test kit in a community telephone sample. J Acquir Immune Defic Syndr. 2000;24(4):363-368. PubMed | Google Scholar
- Hlongwa M, Mashamba-Thompson T, Makhunga S, Muraraneza C, Hlongwana K. Men´s perspectives on HIV self-testing in sub-Saharan Africa: a systematic review and meta-synthesis. BMC Public Health. 2020;20(1):66. PubMed | Google Scholar
- Njau B, Covin C, Lisasi E, Damian D, Mushi D, Boulle A et al. A systematic review of qualitative evidence on factors enabling and deterring uptake of HIV self-testing in Africa. BMC Public Health. 2019;19(1):1289. PubMed | Google Scholar
- Makusha T, Knight L, Taegtmeyer M, Tulloch O, Davids A, Lim J et al. HIV self-testing could “revolutionize testing in South Africa, but it has got to be done properly”: perceptions of key stakeholders. PLoS ONE. 2015;10(3):e0122783. PubMed | Google Scholar
- Van Rooyen H, Tulloch O, Mukoma W, Makusha T, Chepuka L, Knight LC et al. What are the constraints and opportunities for HIVST scale-up in Africa? Evidence from Kenya, Malawi and South Africa. J Int AIDS Soc. 2015;18(1):19445. PubMed | Google Scholar
- Perez GM, Steele SJ, Govender I, Arellano G, Mkwamba A, Hadebe M et al. Supervised oral HIV self-testing is accurate in rural KwaZuluNatal, South Africa. Tropical Med Int Health. 2016;21(6):759-67. PubMed | Google Scholar
- Choko AT, Desmond N, Webb EL, Chavula K, Napierala-Mavedzenge S, Gaydos CA et al. The uptake and accuracy of oral kits for HIV self-testing in high HIV prevalence setting: a cross-sectional feasibility study in Blantyre, Malawi. PLoS Med. 2011;8(10):e1001102. PubMed | Google Scholar
- Madiba S, Mokgatle M. Students want HIV testing in schools” a formative evaluation of the acceptability of HIV testing and counselling at schools in Gauteng and North West provinces in South Africa. BMC Public Health. 2015;15:388. PubMed | Google Scholar
- Merchant RC, Clark MA, Liu T, Rosenberger JG, Romanof J, Bauermeister J et al. Preferences for oral fuid rapid HIV self-testing among social media-using young black, Hispanic, and white men-who-have-sex-with-men (YMSM): implications for future interventions. Public Health. 2017;145:7-19. PubMed | Google Scholar
- Johnson CC, Kennedy C, Fonner V, Siegfried N, Figueroa C, Dalal S et al. Examining the effects of HIV self-testing compared to standard HIV testing services: a systematic review and meta-analysis. J Int AIDS Soc. 2017;20(1):21594. PubMed | Google Scholar
- Pant Pai N, Bhargava M, Joseph L, Sharma J, Pillay S, Bea B. Will an unsupervised self-testing strategy be feasible to operationalize in Canada? Results from a pilot study in students of a large Canadian university. AIDS Res Treat. 2014;2014:747619. PubMed | Google Scholar
- Harichund C, Moshabela M. Acceptability of HIV Self-Testing in Sub-Saharan Africa: Scoping Study. AIDS Behav. 2018;22(2):560-568. PubMed | Google Scholar
- Johnson C, Baggaley R, Forsythe S, van Rooyen H, Ford N, Napierala Mavedzenge S et al. Realizing the potential for HIV self-testing. AIDS Behav. 2014;18(Suppl 4):S391-5. PubMed | Google Scholar
- Musheke M, Ntalasha H, Gari S, Mckenzie O, Bond V, Martin-Hilber A et al. A systematic review of qualitative findings on factors enabling and deterring uptake of HIV testing in Sub-Saharan Africa. BioMed Cent Public Health. 2013;13(220):1-16. PubMed | Google Scholar
- Nyblade L, Stangl A, Weiss E, Ashburn K. Combating HIV stigma in health care settings: what works. J Int AIDS Soc. 2009;12(1):15. PubMed | Google Scholar
- Joint United Nations Programme on HIV/AIDS (UNAIDS). Understanding Fast-Track: Accelerating action to end the AIDS epidemics by 2030. 2015.