Myoma expulsion after embolization: case report and literature review
Maria Clara Amorim Silva, Rafael Everton Assunção Ribeiro da Costa, Wilson de Oliveira Sousa Júnior, Ariane Pereira Carvalho, Sabas Carlos Vieira
Corresponding author: Rafael Everton Assunção Ribeiro da Costa, Health Science Center, State University of Piauí, Teresina (PI), Brazil 
Received: 30 Oct 2022 - Accepted: 13 Nov 2022 - Published: 28 Dec 2022
Domain: Gynecology
Keywords: Myoma, uterine artery embolization, postoperative complications, case report
©Maria Clara Amorim Silva et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Maria Clara Amorim Silva et al. Myoma expulsion after embolization: case report and literature review. Pan African Medical Journal. 2022;43:210. [doi: 10.11604/pamj.2022.43.210.38030]
Available online at: https://www.panafrican-med-journal.com//content/article/43/210/full
Myoma expulsion after embolization: case report and literature review
![]() Maria Clara Amorim Silva1,
Maria Clara Amorim Silva1, ![]() Rafael Everton Assunção Ribeiro da Costa1,&, Wilson de Oliveira Sousa Júnior2,
Rafael Everton Assunção Ribeiro da Costa1,&, Wilson de Oliveira Sousa Júnior2, ![]() Ariane Pereira Carvalho3, Sabas Carlos Vieira4
Ariane Pereira Carvalho3, Sabas Carlos Vieira4
&Corresponding author
Uterine artery embolization (UAE) is a very efficient treatment modality for myoma. A rare complication of this procedure is vaginal expulsion of the uterine myoma (expelled myoma) which may occur in 3 to 5% of cases during a period of 3 to 48 months. We report a case of myoma expulsion after embolization, discussing diagnosis and treatment. A literature review was also conducted. A 40-year-old patient sought medical care on 5/2/2021 with intermittent pelvic pain and hypermenorrhagia. Vaginal ultrasound revealed an enlarged uterus (253 cm3) with myomas. The largest intramural myoma measured 7 cm. Uterine artery embolization was performed on 11/11/2021, without any complications. On 12/7/2021, during clinical examination an expelled myoma was observed entirely inside the vaginal canal. A vaginal myomectomy was performed, without any complications. At 15 months after the initial follow-up, the patient is doing well.
Uterine artery embolization (UAE) is an effective treatment for symptomatic myomas since 1995 and symptom resolution occurs in 85-95% of cases [1,2]. Ideal candidates for the procedure are patients who wish to preserve their uterus, have no desire to conceive and those experiencing dysmenorrhea or hypermenorrhagia, in addition to premenopausal women [3]. As a result, ischemia, decreased myoma size occur, and endometrial perfusion is maintained. Finally, myoma remnants are absorbed by the preserved myometrium [1]. Nevertheless, a rare and late complication that merits discussion with candidates to UAE is vaginal expulsion of the uterine myoma (expelled myoma). The incidence of this complication is 3 to 5% of cases in a period of 3 to 48 months. It causes discomfort and requires surgical treatment. The process is due to uterine contractions secondary to the secretion of inflammatory prostaglandins, owing to the presence of necrotic material in the uterine cavity. Pedunculated submucosal myoma is the most common type of expelled myoma. Treatment of this complication requires antimicrobial coverage and the removal of all necrotic material by means of laparotomy, laparoscopy, hysteroscopy and/or hysterectomy to prevent sepsis [1].
The aim of this study is to report a case of myoma expulsion after embolization. The aspects of diagnosis and treatment were addressed and a literature review was also conducted.
Patient information: on 5/2/2021, a 40-year-old patient sought medical care, complaining of intermittent pelvic pain and hypermenorrhagia, that lasted up to 4 days. Systemic repercussions resulted in adynamia. The patient was a G0P0A0 woman and had no other comorbidities.
Clinical findings: on clinical examination, the uterus was palpable at about 4 cm from the symphysis pubis. Mucosae were pale +/4+ and no other alterations were observed.
Diagnostic assessment: transvaginal ultrasonography (TVUS) demonstrated an enlarged uterus (253 cm3) with the presence of myomas. The largest myoma measured 7 cm (intramural location). Hemoglobin and hematocrit levels were 8.5 and 29.2, respectively. As a result of these findings, oral iron replacement and laparoscopic myomectomy were indicated. After these indications, the patient chose embolization, since she had no reproductive desire and wished to preserve the uterus. Magnetic resonance imaging (MRI) of the pelvis was performed (Figure 1 A), revealing the presence of uterine myomas. The largest submucosal myoma measured 9 x 8.8 cm and there was also an intramural component. Total uterine volume was 597 cm3. Figure 1 B shows pelvic MRI scan performed after the embolization procedure.
Therapeutic interventions: selective embolization of the uterine arteries was performed on 11/11/2021. Access was achieved via unilateral right femoral artery, using catheters and the injection of embolizing agents (microparticles of polyvynil alcohol). Uterine artery embolization procedure was performed under general anesthesia. The technique was successful and the patient was discharged from the hospital on the second postoperative day with minimal vaginal bleeding.
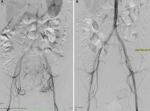
Follow-up and outcome of interventions: in the three following weeks, the patient sought the emergency department with complaints of pain. On the 25th day after surgery, she began to feel vaginal discomfort with the sensation of mass externalization. Figure 2 shows the angiography performed before (Figure 2 A) and after (Figure 2 B) UAE. On 11/18/2021, the patient experienced intense pelvic abdominal pain, seeking urgent medical care. Abdominal computed tomography (CT) scan showed an image suggestive of hematometrium of around 240mL. She was medicated with analgesics with partial pain improvement. A new pelvic MRI was performed, revealing myoma devascularization. On 12/7/2021, she reported intense colicky pelvic pain and the sensation of a mass being eliminated through the vagina. On clinical exam, an expelled myoma was located entirely within the vaginal canal (Figure 3 A). The patient was transported to the operating room, where vaginal myomectomy was performed under subarachnoid anesthesia without any complications. The surgical specimen was shown in Figure 3 B. She was discharged from the hospital after 48 hours, maintaining treatment with iron replacement, tranexamic acid and ciprofloxacin for 7 days. On 12/18/2021, a levonorgestrel intrauterine device (IUD) was inserted into the uterus of the patient. Histopathology study of the surgical specimen confirmed that it was a necrotic leiomyoma. On 01/14/2022, since breakthrough bleeding persisted, an oral dienogest was combined for two months. At 15 months after the initial follow-up visit, the patient is currently asymptomatic and has a better quality of life.
Diagnosis: myoma expulsion after embolization.
Informed consent: this study was approved by the Institutional Review Board of the State University of Piauí, Teresina (PI), Brazil - reference number 5.535.238 (CAAE: 59331922.7.0000.5209). The patient signed the informed consent form (ICF).
Uterine leiomyomas are common benign tumors that usually occur in women over the age of 35. The most frequently reported symptoms are abnormal uterine bleeding (menometrorrhagia) and pelvic compression, occurring in about 20% of women [4,5]. UAE is a procedure in which the uterine arteries are embolized and the myoma is devascularized. Uterine size is also reduced. The technique has several advantages over hysterectomy (definitive treatment that prevents recurrences). UAE is a minimally invasive, well-tolerated, effective treatment modality that has lower complication rates and a shorter postoperative period [4,6]. It can also be performed in patients with absolute or relative contraindications to surgery, e.g. severe cardiopulmonary disease and thromboembolism, in addition to locally advanced pelvic cancers with active bleeding [6].
The majority of complications of UAE described in the literature are not life-threatening. Most patients experience only mild symptoms such as fever, pain and nausea [7]. Myoma expulsion is a rare complication. It can lead to endometritis and sepsis, which require rapid identification and treatment [5]. In the PubMed database, using the words myoma, embolization and expulsion, we found only 18 cases reported in the literature (Table 1) [2,3,5,7-14]. Initial treatment included intravenous fluids, antibiotics and curettage of necrotic remnants within the endometrial cavity. In the lack of response, hysterectomy is required to prevent patient risk [5]. When this diagnosis is suspected, MRI has significant value due to its higher sensitivity. It is also the imaging modality of choice before and after UAE, since it identifies the size, position and number of myomas in the uterine cavity [6].
During myoma expulsion, which may consist of prolonged periods of desquamation, patients may experience symptoms ranging from minimal discomfort to vaginal discharge, bleeding and low fever. In a study by Kroencke et al. data was validated according to a patient report [13]. She described that desquamation was part of the expulsion process and occurred for 7 months after UAE [7]. Regarding contraindications, myomas larger than 10 cm and submucosal myomas do not invalidate the performance of the procedure. Although there is a higher association between complications and larger myomas, complications most likely arise from the location rather than the size of the myoma [5]. In contrast, a successful procedure is defined as improvement in symptoms and no need for further treatment. In addition, the reduction in uterine size varies from 40 to 70% after undergoing the procedure [7].
The effects of UAE on women suffering from infertility and abortions are still not fully known. Ravina et al. conducted a study showing unplanned pregnancy in twelve women after undergoing the technique, with 58.3% occurring in women over 37 years of age. This study proved that conception was facilitated by decreasing the amount of myomas and restoring normal uterine configuration [2,7,15].
In this study, the case report described a 40-year-old woman, within the mean age (43.5 years) calculated in the 11 case studies published in the literature, as shown in Table 1. In this case, it is worth mentioning that after the procedure the only minor complication was pain, which is considered a common symptom. In the presence of a protruding mass, the procedure of choice was hysteroscopy for removal of necrotic material. The patient had a good response to hormone treatment, with resolution of menstrual bleeding.
Myoma expulsion after UAE has not been commonly reported in the literature. To the best of our knowledge, only 18 cases have been described in the literature to date. Most of these patients were treated with analgesics and antibiotics, in addition to the removal of necrotic remnants by means of a simple procedure - hysteroscopy with curettage. Nevertheless, in severe cases due to failure of myometrial perfusion, hysterectomy is the treatment of choice.
The authors declare no competing interests.
Maria Clara Amorim Silva and Rafael Everton Assunção Ribeiro da Costa contributed to study concept, data curation, formal analysis, project management and writing (original draft, review and editing); Wilson de Oliveira Sousa Júnior, Ariane Pereira Carvalho and Sabas Carlos Vieira contributed to study concept, data curation, formal analysis, project management and writing (review and editing). All the authors read and approved the final version of this manuscript.
Table 1: case studies described in the literature of myoma expulsion following UAE, according to author, year, number of cases, age (mean, in years), reason for UAE, post-UAE complications and procedures
Figure 1: A) MRI before embolization (sagittal post contrast T1 fat saturation image demonstrated intense contrast enhancement of the myoma); B) MRI after embolization (sagittal post contrast T1 fat saturation image); it was observed that the myoma was no longer contrast-enhanced after embolization and its dimensions decreased
Figure 2: A) angiography before embolization showing uterine hypervascularization; B) angiography after embolization showing a devascularized myoma
Figure 3: A) myoma externalized through the vagina; B) expelled myoma specimen
- Kim KA, Yoon SW, Yoon BS, Park CT, Kim SH, Lee JT. Spontaneous vaginal expulsion of uterine myoma after magnetic resonance-guided focused ultrasound surgery. J Minim Invasive Gynecol. 2011;18(1):131-134. PubMed | Google Scholar
- Laverge F, D'Angelo A, Davies NJ, Wood A, Amso NN. Spontaneous expulsion of three large fibroids after uterine artery embolization. Fertil Steril. 2003;80(2):450-452. PubMed | Google Scholar
- do Amaral VF, Yochiy FY, Furlanetto ML Jr, Payão SLM. Myoma Expulsion after Uterine Artery Embolization. Case Rep Surg. 2021;2021:6644229. PubMed | Google Scholar
- Bérczi V, Valcseva É, Kozics D, Kalina I, Kaposi P, Sziller P et al. Safety and Effectiveness of UFE in Fibroids Larger than 10 cm. Cardiovasc Intervent Radiol. 2015;38(5):1152-1156. PubMed | Google Scholar
- Martins JG, Gaudenti D, Crespo F, Ganesh D, Verma U. Uncommon Complication of Uterine Artery Embolization: Expulsion of Infarcted Myoma and Uterine Sepsis. Case Rep Obstet Gynecol. 2016;2016:8695318. PubMed | Google Scholar
- Huang LY, Cheng YF, Huang CC, Chang SY, Kung FT. Incomplete vaginal expulsion of pyoadenomyoma with sepsis and focal bladder necrosis after uterine artery embolization for symptomatic adenomyosis: case report. Hum Reprod. 2003;18(1):167-171. PubMed | Google Scholar
- Felemban A, Stein L, Tulandi T. Uterine restoration after repeated expulsion of myomas after uterine artery embolization. J Am Assoc Gynecol Laparosc. 2001;8(3):442-444. PubMed | Google Scholar
- Marret H, Keris Yle B, Acker O, Cottier JP, Herbreteau D. Late leiomyoma expulsion after uterine artery embolization. J Vasc Interv Radiol. 2004;15(12):1483-1485. PubMed | Google Scholar
- Hehenkamp WJ, Volkers NA, Van Swijndregt AD, De Blok S, Reekers JA, Ankum WM. Myoma expulsion after uterine artery embolization: complication or cure? Am J Obstet Gynecol. 2004;191(5):1713-1715. PubMed | Google Scholar
- Redecha M Jr, Holomán K, Javorka V, Mizícková M, Ferianec V, Papcun P et al. Myoma expulsion after uterine artery embolization. Arch Gynecol Obstet. 2009;280(6):1023-1024. PubMed | Google Scholar
- Park HR, Kim MD, Kim NK, Kim HJ, Yoon SW, Park WK et al. Uterine restoration after repeated sloughing of fibroids or vaginal expulsion following uterine artery embolization. Eur Radiol. 2005 Sep;15(9):1850-4. PubMed | Google Scholar
- Pollard RR, Goldberg JM. Prolapsed cervical myoma after uterine artery embolization. A case report. J Reprod Med. 2001;46(5):499-500. PubMed | Google Scholar
- Kroencke TJ, Gauruder-Burmester A, Enzweiler CN, Taupitz M, Hamm B. Disintegration and stepwise expulsion of a large uterine leiomyoma with restoration of the uterine architecture after successful uterine fibroid embolization: case report. Hum Reprod. 2003;18(4):863-865. PubMed | Google Scholar
- Abbara S, Spies JB, Scialli AR, Jha RC, Lage JM, Nikolic B. Transcervical expulsion of a fibroid as a result of uterine artery embolization for leiomyomata. J Vasc Interv Radiol. 1999;10(4):409-411. PubMed | Google Scholar
- Ravina JH, Vigneron NC, Aymard A, Le Dref O, Merland JJ. Pregnancy after embolization of uterine myoma: report of 12 cases. Fertil Steril. 2000;73(6):1241-1243. PubMed | Google Scholar
Search
This article authors
On Pubmed
On Google Scholar
Citation [Download]
Navigate this article
Similar articles in
Key words
Tables and figures
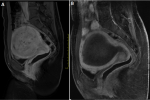 Figure 1: A) MRI before embolization (sagittal post contrast T1 fat saturation image demonstrated intense contrast enhancement of the myoma); B) MRI after embolization (sagittal post contrast T1 fat saturation image); it was observed that the myoma was no longer contrast-enhanced after embolization and its dimensions decreased
Figure 1: A) MRI before embolization (sagittal post contrast T1 fat saturation image demonstrated intense contrast enhancement of the myoma); B) MRI after embolization (sagittal post contrast T1 fat saturation image); it was observed that the myoma was no longer contrast-enhanced after embolization and its dimensions decreased