Baclofen and catatonia: a case report
Jamir Pitton Rissardo, Sai Nikhil Konduru, Vinay Kumar Gadamidi, Ana Letícia Fornari Caprara
Corresponding author: Jamir Pitton Rissardo, Medicine Department, Federal University of Santa Maria, Santa Maria, Brazil 
Received: 01 Dec 2022 - Accepted: 13 Dec 2022 - Published: 21 Dec 2022
Domain: Neurology (general)
Keywords: Baclofen, lioresal, catatonia, psychosis, case report
©Jamir Pitton Rissardo et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Jamir Pitton Rissardo et al. Baclofen and catatonia: a case report. Pan African Medical Journal. 2022;43:198. [doi: 10.11604/pamj.2022.43.198.38403]
Available online at: https://www.panafrican-med-journal.com//content/article/43/198/full
Baclofen and catatonia: a case report
Jamir Pitton Rissardo1,&, ![]() Sai Nikhil Konduru2,
Sai Nikhil Konduru2, ![]() Vinay Kumar Gadamidi3,
Vinay Kumar Gadamidi3, ![]() Ana Letícia Fornari Caprara1
Ana Letícia Fornari Caprara1
&Corresponding author
Baclofen was approved for medical use in the United States in 1977 by Food and Drug Administration. Serious adverse effects associated with this medication are uncommon at usually prescribed doses. Herein, we present a case of baclofen-induced catatonia in a young-adult female with back pain receiving oral baclofen. A 20-year-old female presented to the emergency department with possible seizure-like activity. It was reported that the patient was suffering from acute back pain and was prescribed baclofen three times a day by her general physician one day before her presentation. Upon further discussion, it was known that following an altercation with her family member, she had attempted suicide by consuming 200 mg of baclofen and then developed rapidly progressive symptoms of aphasia, mutism, and decreased oral intake. Laboratory tests, cerebrospinal fluid analysis, and neuroimaging were unremarkable. Electroencephalogram was normal. Bush-Francis Catatonia Rating Scale score was 27. She showed significant improvement following low-dose lorazepam administration. There are four reports in the literature of catatonia secondary to baclofen. The present report is the first to describe the occurrence of catatonia in a previously healthy individual. Analysis of these cases suggests a relationship between a history of psychotic symptoms and catatonia. All the reports were classified as probable by the Naranjo algorithm.
Baclofen was approved for medical use in the United States in 1977 by Food and Drug Administration. Interestingly, baclofen was initially developed for managing epilepsy. But this drug showed no significant effect on the control of seizure activity. During the 1970s, several animal studies demonstrated good efficacy of baclofen for treating muscle spasticity [1].
Baclofen can be used in many conditions, including spastic paralysis, traumatic spinal injury, stroke, and multiple sclerosis. Also, this muscle relaxant has several off-label uses, such as persistent and chronic hiccups. Some available baclofen dosage forms are oral, transdermal, and intrathecal administration through pump infusion. Serious adverse effects associated with this medication are uncommon at usually prescribed doses. However, baclofen overdose was already related to severe neurological side effects like delirium, seizures, and coma [2]. In this context, baclofen was rarely associated with catatonia, potentially life-threatening muscle spasticity characterized by mutism, posturing, rigidity, and withdrawal. Herein, we present a case of baclofen-induced catatonia in a young-adult female with back pain receiving oral baclofen.
Patient information: a 20-year-old female presented to the emergency department with possible seizure-like activity. She was previously healthy, and her family history was unremarkable for neuropsychiatric conditions.
Clinical findings: upon initial evaluation, she was observed to have abnormal posture, facial expression, and stereotypical movements. She was awake but nonverbal with minimal resistance and combativeness.
Timeline of current episode: her father reported that she complained of acute back pain the day before the presentation, and her general practitioner prescribed baclofen three times a day. Upon further discussion, it was known that following an altercation with her family member, she had attempted suicide by consuming 200 mg of baclofen and then developed rapidly progressive symptoms of aphasia, mutism, and decreased oral intake. The patient was brought to the emergency department by family members the day after the onset of symptoms.
Diagnostic assessment: she was admitted to the hospital and underwent an extensive workup that included a complete blood count, liver function test, metabolic panel, urine analysis/culture, and sexually transmitted serologies, all of which were within normal limits. An electrocardiogram revealed normal sinus rhythm and a QT interval of 350ms. A lumbar puncture was performed, and cerebrospinal fluid analysis was normal. A cranial computed tomography scan was negative. Brain magnetic resonance imaging was unremarkable, without any acute process and signs of encephalitis. Because of her seizure-like activity, an electroencephalogram was performed and revealed normal background for her age without any epileptic activity.
Diagnosis: her symptom and negative workup indicated that physical and mental status examinations were associated with catatonia. Bush-Francis Catatonia Rating Scale (CRS) was remarkable for catatonia, and significant symptoms like stupor, mutism, withdrawal, and staring were noted. She was negative for autonomic stability, hyperactivity, echolalia, and impulsivity.
Therapeutic interventions: she showed significant improvement following low-dose lorazepam (3mg/day in divided doses orally) administration.
Follow-up and outcome of interventions: initially, her motor and stereotyped movements started to improve. On the third day of hospitalization, she was asymptomatic. During the remaining of her hospitalization, she demonstrated no signs of catatonia. She remained nonrigid, well-versed, and eating adequately. At one and three months, she spoke fluently and moved all extremities. No episodes of psychosis, depression, or mania were observed in long-term follow-up.
Patient perspective: “I felt that I was trapped inside my body”.
Informed consent: a written consent form was obtained from the patient for this publication.
Catatonia is a neuropsychiatric syndrome characterized by abnormal movements, behaviors, and withdrawal. A physical and mental assessment of the present individual displayed signs like stupor, mutism, staring, rigidity, withdrawal, and posturing, supporting the diagnosis of catatonia. Catatonia was assessed using Bush-Francis Catatonia Rating Scale (CRS), and her score was 27. Significant improvement in the motor symptoms following the administration of a benzodiazepine can further support the diagnosis of catatonia [3].
Baclofen, also known as 4-Amino-3-(4-chlorophenyl) butanoic acid, is a lipophilic analog of γ-aminobutyric acid (GABA). The baclofen´s mechanism of action is not fully understood. It is believed that this drug is an agonist of the beta subunit of GABA for mono and polysynaptic neurons in the spinal cord and brain. In this way, baclofen probably reduces spasticity by stimulating inhibitory neuronal signals in the post-synaptic neurons and also reduces the release of excitatory neurotransmitters at the presynaptic neurons [1]. Interestingly, intrathecal baclofen is preferred when the patients are unresponsive to oral therapy, mainly in cases of traumatic brain injury and spinal cord lesions. Baclofen´s abrupt discontinuation can cause seizures and hallucinations [4]. This baclofen withdrawal syndrome is important because it supports the hypothesis that baclofen would have a cortical action.
Baclofen-induced catatonia was rarely reported in the literature. It is worth mentioning that the clinical trial for baclofen approval did not record any patient with catatonic symptoms. A literature search was performed in Google Scholar and Medline/PubMed using a set of terms that included baclofen and catatonia (Table 1) [2,4-6]. Analysis of these cases suggests a relationship between a history of psychotic symptoms and catatonia. All the reports were classified as probable by the Naranjo algorithm [7]. Patients with baclofen-induced catatonia usually present with major clinical manifestations of catatonia, such as mutism, stupor, and rigidity. Pauker and Brown highlighted the role of multiple components influencing catatonic symptoms [5]. They suggested a possible interaction among drugs contributed to the development of catatonia.
Baclofen doses of more than 200 mg are associated with coma, delirium, and seizures. Toxicologic studies revealed a clinical spectrum of baclofen overdose involving encephalopathy, respiratory depression, muscular hypotonia, and generalized hyporeflexia. Interestingly, this was mainly observed in individuals with renal impairment. Nahar et al. reported a patient with catatonic features in addition to psychosis following a baclofen overdose [2]. Psychosis with catatonic features was already described with other muscle relaxants. In 1983, Beeber and Manring probably depicted the first case of catatonia secondary to a muscle relaxant [8]. They reported a 38-year-old female who received cyclobenzaprine for back pain. She developed manic psychosis and some catatonic symptoms (posturing and echolalia). Noteworthy, the patient had a previous significant psychiatric medical history, including manic episodes.
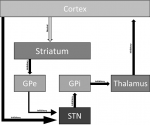
A possible explanation for baclofen-induced catatonia is the interaction of baclofen in GABA receptors in the basal ganglia (Figure 1). The motor control involves GABAergic and glutamatergic neurons in the cortico-striato-pallido-thalamo-cortical loop. In this way, the increased GABAergic activity can lead to direct or indirect inhibition of dopamine release. This modulation of firing dopamine neurons could contribute to developing psychotic and motor symptoms characteristic of catatonia [9]. Moreover, mania-like symptoms can be explained by an increased noradrenergic turnover by altering the firing rate of GABAergic neurons [10]. Another hypothesis is serotoninergic disinhibition, which can partially explain some mania-related symptoms. It is believed that presynaptic GABA-B receptors interaction in the dorsal raphe nucleus can increase serotonin release [3].
A more recent hypothesis for explaining catatonia involves a disbalance between GABA receptors. In rat models, it was observed that hyperactivity at the GABA-B receptor and hypoactivity at the GABA-A receptor could cause catatonia symptoms [9]. In this context, baclofen may lead to increased selective activity of GABA-B receptors in susceptible individuals [1]. It is worth mentioning that this pathway can explain hypokinetic catatonia but does not explain exciting types of catatonia. To be more specific, borderline forms like periodic catatonia and delirious mania are not supported by this pathophysiological mechanism [9].
Catatonia secondary to baclofen was rarely reported in the literature. Most of the affected patients have a previous medical history of psychotic symptoms and catatonia. The mechanism for explaining baclofen-induced catatonia probably involves increased GABAergic neurotransmission or a disbalance between different GABA receptors. Clinicians should be aware of this possible side effect to prompt diagnosis and short-term recovery.
The authors declare no competing interests.
Patient management, data collection, and manuscript drafting: Jamir Pitton Rissardo; manuscript revision: Sai Nikhil Konduru, Vinay Kumar Gadamidi, Ana Letícia Fornari Caprara. All the authors read and approved the final version of this manuscript.
Table 1: literature review of catatonia associated with baclofen
Figure 1: possible pathophysiological mechanism for baclofen-induced catatonia
- Romito JW, Turner ER, Rosener JA, Coldiron L, Udipi A, Nohrn L et al. Baclofen therapeutics, toxicity, and withdrawal: A narrative review. SAGE Open Med. 2021 Jun 3;9:20503121211022197. PubMed | Google Scholar
- Nahar A, Shanker Reddy MS, Subramaniyam BA, Thippeswamy H, Chandra PS, Chaturvedi SK. Baclofen Overdose Presenting as Psychosis with Catatonia. Indian J Psychol Med. 2017 Sep-Oct;39(5):695-697. PubMed | Google Scholar
- Jaimes-Albornoz W, Ruiz de Pellon-Santamaria A, Nizama-Vía A, Isetta M, Albajar I, Serra-Mestres J. Catatonia in older adults: A systematic review. World J Psychiatry. 2022 Feb 19;12(2):348-367. PubMed | Google Scholar
- Shaw B, Thapa P, Reeves M. Catatonia Associated with Intrathecal Baclofen: A Case Report. Psychiatric Ann. 2022 Feb;52(2):85-7. Google Scholar
- Pauker SL, Brown R. Baclofen-induced catatonia. J Clin Psychopharmacol. 1986 Dec;6(6):387-8. PubMed | Google Scholar
- Dcruz M, Mahadevan J, Chand P, Murthy P. An interesting presentation of psychotic catatonia in an elderly patient with alcohol dependence. J Geriatr Ment Health. 2019 Oct;6(2):101-3. Google Scholar
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981 Aug;30(2):239-45. PubMed | Google Scholar
- Beeber AR, Manring JM Jr. Psychosis following cyclobenzaprine use. J Clin Psychiatry. 1983 Apr;44(4):151-2. PubMed | Google Scholar
- Walther S, Stegmayer K, Wilson JE, Heckers S. Structure and neural mechanisms of catatonia. Lancet Psychiatry. 2019 Jul;6(7):610-619. PubMed | Google Scholar
- Yu X, Ba W, Zhao G, Ma Y, Harding EC, Yin L et al. Dysfunction of ventral tegmental area GABA neurons causes mania-like behavior. Mol Psychiatry. 2021 Sep;26(9):5213-5228. PubMed | Google Scholar