A recurrent side-changing febrile pleural effusion revealing familial Mediterranean fever: a case report
Islam Mejri, Asma Saidane, Nouha Boubaker, Samira Mhamdi, Selsabil Daboussi, Chiraz Aichaouia, Zied Moatemri
Corresponding author: Islam Mejri, Military Hospital, Department of Pulmonology, Tunis, Tunisia 
Received: 17 Jan 2022 - Accepted: 20 Oct 2022 - Published: 03 Nov 2022
Domain: Internal Medicine, Pulmonology
Keywords: Familial Mediterranean fever, fever, pleural effusion, familial Mediterranean fever gene, case report
©Islam Mejri et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Islam Mejri et al. A recurrent side-changing febrile pleural effusion revealing familial Mediterranean fever: a case report. Pan African Medical Journal. 2022;43:121. [doi: 10.11604/pamj.2022.43.121.33324]
Available online at: https://www.panafrican-med-journal.com//content/article/43/121/full
Case report 
A recurrent side-changing febrile pleural effusion revealing familial Mediterranean fever: a case report
A recurrent side-changing febrile pleural effusion revealing familial Mediterranean fever: a case report
![]() Islam Mejri1,2,&, Asma Saidane1, Nouha Boubaker1, Samira Mhamdi1,2, Selsabil Daboussi1,2, Chiraz Aichaouia1,2,
Islam Mejri1,2,&, Asma Saidane1, Nouha Boubaker1, Samira Mhamdi1,2, Selsabil Daboussi1,2, Chiraz Aichaouia1,2, ![]() Zied Moatemri1,2
Zied Moatemri1,2
&Corresponding author
Familial Mediterranean Fever (FMF), characterized by recurrent polyserositis, is an autosomal recessive disease involving essentially Mediterranean populations. We report the case of a 30-year-old Tunisian military patient complaining of fever and chest pain recurring on board a Navy military vessel, due to side-changing pleural effusion. On landing, a marked improvement of symptoms was noticed. Gene testing was performed when the diagnostic survey ruled out common etiologies, revealing a homozygous mutation of the FMF gene type M680l/M680l. The prescription of colchicine and the exemption from boarding led to the resolution of the symptoms with no recurrence of pleural effusion. Therefore, the diagnosis of FMF should be considered in a context of a recurrent pleural effusion in the youth, with a negative etiological assessment, notably in an ethnic group at risk. Thus, early diagnosis and adequate treatment may prevent the development of secondary amyloidosis, a serious complication of FMF.
Familial Mediterranean Fever (FMF) is the most common inherited auto-inflammatory disease [1]. It results in recurrent acute attacks of febrile polyserositis (peritonitis, arthritis, pleurisy…). Pleural effusion and fever are the only symptoms of the disease in 5-10% of patients [2]. We report a case of recurrent, febrile, self-resolving pleural effusion in a Tunisian military Navy officer confirmed by a genetic screen.
Patient information: a 30-year-old nonsmoker patient was referred to our pulmonology department. He was operating in the Tunisian marine Navy with no significant personal or familial past medical history. He complained of left-sided chest pain having started 10 days ago, with dyspnea on exertion and diffuse arthralgia. A similar episode occurred six months ago on board the Navy vessel, treated empirically with antibiotics and corticosteroids.
Clinical findings: physical examination was normal except for left-sided pleuretic syndrome. The chest X-ray revealed a minimal left-sided pleural effusion (Figure 1). The contrast-enhanced chest-computer tomography showed a mild pleural fluid in the left chest, without any parenchymal involvement, and ruled out embolism (Figure 2). Nevertheless, a pleural puncture or biopsy could not be performed because of the rapid regression of the effusion.
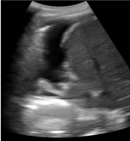
Timeline of current episode: at the time, the patient had received an antibiotic (Amoxicillin-clavulanic acid) without any proof of infection for 7 days. After a partial clinical and radiological improvement, he was discharged. Four months later, he was admitted for recurrence of the chest pain on the contralateral side, with vomiting and mild fever (+38°C). No abdominal pain was reported. The chest X-Ray showed a minimal right-sided pleural effusion. The chest ultrasound confirmed the presence of a minimal right-sided hypoechoic unloculated pleurisy (Figure 3).
Diagnostic assessment: laboratory investigations revealed a leukocytosis (10400/mm3) and an elevated C-reactive protein (CRP) (221 mg/l). The renal test didn't show any microscopic hematuria or proteinuria. The tuberculin skin test and immunological screen were negative. Serum protein electrophoresis was normal. The echocardiography and abdominal ultrasound were normal.
Diagnosis: the diagnosis of familial Mediterranean fever was considered by, in light of: recurrent, febrile, self-resolving episodes of a side-changing pleural effusion and arthralgia, without any underlying cause that could explain these attacks. The genetic testing showed a homozygous mutation of the Mediterranean Fever (MFEV) gene type (M680I/M680I).
Therapeutic interventions: colchicine was initiated at a dosage of 1 mg daily with an immediate improvement. Besides, we referred our patient to an occupational physician for professional redeployment, to prevent the recurrence of further attacks. Screening the family members identified similar asymptomatic cases in the brotherhood.
Follow-up and outcome of interventions: six months and one year later, he was seen on routine follow-up. He was asymptomatic, without any evidence of pleural or pericardial effusion.
Patient perspective: "I feel relieved since I have a diagnosis for my symptoms. Currently, I know how to manage my illness and relieve my pain". "Since I have been on medication, I have a better quality of life with no pain or discomfort". "I am now sensitizing my family to screen this disease".
Informed consent: written consent was obtained from the patient to publish images and clinical information relating to the case. The patient consented to his clinical information except name to be published to contribute to science and global health.
Familial Mediterranean fever is an auto-inflammatory autosomal recessive disease, affecting mainly people of Mediterranean ancestry (Sephardic Jews, Arabs, Armenian…). The main locations of the disease are (the peritoneum, the synovium, the joints...). However, the pleural or the pericardial involvement remains uncommon [3]. We report a case of a Tunisian marine officer diagnosed with FMF revealed by recurrent febrile episodes of side-changing pleural effusion. The diagnosis was challenging in our case, especially in the absence of a positive family history of FMF or consanguinity. This disease may be responsible for a wide spectrum of symptoms (chest pain, fever, arthralgia…). Our study case complained of fever, chest pain, and dyspnea. Acute attacks may be triggered by many factors: infections, stress, intense physical activity, extreme variation of temperatures and menstruation [4]. Our patient has worked as a marine for years in a Mediterranean region (Tunisia). Extreme climatic changes and hard physical activity could have precipitated these acute episodes. Laboratory tests may show an increased level of acute inflammation proteins (CRP, Fibrinogen, and Interleukin 6…). We did not find any underlying infection in our case that could explain these recurrent attacks. Imaging may objectify pleural thickening or minimal pleural plaques due to the recurrence of acute inflammatory attacks. The pleural biopsy may show a chronic, non-specific inflammation. However, it was not performed in our case because of the small amount of the effusion and its rapid regression.
Familial Mediterranean fever, also known as «recurrent polyserositis» or «the periodic disease» is a genetic condition due to a mutation of the MFEV gene located in the short arm of the chromosome 16 which encodes for a regulatory protein called «Pyrin», involved in the systemic inflammatory process [5]. Recent studies suggest that genetic haplotypes may have a prognostic value [6]. In our case, the mutation of MFEV gene, at exon 10 type (M680I/M680I), is known to be associated with a greater risk of secondary amyloidosis and worse outcomes. Besides, Frederici et al. have suggested that patients with 2-high homozygous mutation alleles (M680I) develop the disease earlier and are quite more symptomatic with more severe complications as well, than those with one mutation allele (M680I) [7].
Genetic testing may be useful in such atypical cases. However, it is not mandatory. In fact, the FMF is a clinical condition. Many scores have been found to help clinicians assess the diagnosis of FMF, such as the «Tel-Hashomer diagnostic criteria» [8]. Global management aims to prevent further attacks and the silent deposition of Amyloid substances. Colchicine is the mainstream of the treatment. It should be given orally at a dosage of (1-2mg daily). Our patient has completely responded to an adequate dose of Colchicine therapy. In case of resistance, numerous treatments have been tested such as Immunosuppressive drugs (TNF-Alpha Inhibitor, Thalidomid…) and Immunomodulators (Interleukin1 Beta Inhibitor, Etanercept…) [9]. Further researches are required to better understand the underlying mechanisms of this disease and to find out new insights for adequate treatments.
This is a rare case of FMF revealed by recurrent pleural effusion confirmed by genetic testing. The early diagnosis led to the relief of symptoms in our patient and to reveal undiagnosed new cases in his family. Our case report highlights the importance of early screening and treatment of this disease, in order to prevent further attacks and the development of secondary amyloidosis.
The authors declare no competing interests.
Islam Mejri: patient management, data collection and analysis, manuscript writing and revision. Asma Saidane and Nouha Boubaker: manuscript writing. Samira Mhamdi, Selsabil Daboussi and Chiraz Aichaouia: manuscript revision. Zied Moatemri: patient management and manuscript revision. All the authors have read and agreed to the final manuscript.
We thank the patient who accepted to share these data and the Genetic Lab (Hedi Chaker Hospital, Tunisia) who performed the Molecular Screening for FMF.
Figure 1: chest radiography showing minimal left-sided pleural effusion
Figure 2: thorax computed tomography showing left-sided pleural thickening
Figure 3: ultrasound showing minimal right-sided pleural effusion
- Sohar E, Gafni J, Pras M, Heller H. Familial Mediterranean fever. A survey of 470 cases and review of the literature. Am J Med. 1967 Aug;43(2):227-53. PubMed | Google Scholar
- Sever F, Sever M, Sanal S, Yalçin M, Berdeli A. Familial Mediterranean fever with pulmonary manifestations alone; early diagnosis with genetic analysis. Tuberk Toraks. 2012;60(4):380-4. PubMed | Google Scholar
- Tufan A, Lachmann HJ. Familial Mediterranean fever, from pathogenesis to treatment: a contemporary review. Turk J Med Sci. 2020 Nov 3;50(SI-2):1591-1610. PubMed | Google Scholar
- Bhatt H, Cascella M. Familial Mediterranean Fever. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. PubMed | Google Scholar
- Cazeneuve C, Sarkisian T, Pêcheux C, Dervichian M, Nédelec B, Reinert P et al. MEFV-Gene analysis in armenian patients with Familial Mediterranean fever: diagnostic value and unfavorable renal prognosis of the M694V homozygous genotype-genetic and therapeutic implications. Am J Hum Genet. 1999 Jul;65(1):88-97. PubMed | Google Scholar
- Van Gorp H, Huang L, Saavedra P, Vuylsteke M, Asaoka T, Prencipe G et al. Blood-based test for diagnosis and functional subtyping of familial Mediterranean fever. Ann Rheum Dis. 2020 Jul;79(7):960-968. PubMed | Google Scholar
- Federici S, Sormani MP, Ozen S, Lachmann HJ, Amaryan G, Woo P et al. Evidence-based provisional clinical classification criteria for autoinflammatory periodic fevers. Ann Rheum Dis. 2015 May;74(5):799-805. PubMed | Google Scholar
- Kilic A, Varkal MA, Durmus MS, Yildiz I, Yildirim ZNY, Turunc G et al. Relationship between clinical findings and genetic mutations in patients with familial Mediterranean fever. Pediatr Rheumatol Online J. 2015 Dec 12;13:59. PubMed | Google Scholar
- El Hasbani G, Jawad A, Uthman I. Update on the management of colchicine resistant Familial Mediterranean Fever (FMF). Orphanet J Rare Dis. 2019 Oct 15;14(1):224. PubMed | Google Scholar