Prognostic value of Epstein-Barr virus DNA load in nasopharyngeal carcinoma: a meta-analysis
Imane EL Alami, Amina Gihbid, Hicham Charoute, Wafaa Khaali, Selma Mohamed Brahim, Nezha Tawfiq, Rachida Cadi, Khalid Belghmi, Mohammed El Mzibri, Meriem Khyatti
Corresponding author: Meriem Khyatti, Laboratory of Viral Oncology, Institut Pasteur du Maroc, Casablanca, Morocco 
Received: 20 Mar 2021 - Accepted: 02 Jul 2021 - Published: 03 Jan 2022
Domain: Virology
Keywords: Epstein-Barr virus, nasopharyngeal carcinoma, Epstein Barr Virus DNA load, prognostic
©Imane EL Alami et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Imane EL Alami et al. Prognostic value of Epstein-Barr virus DNA load in nasopharyngeal carcinoma: a meta-analysis. Pan African Medical Journal. 2022;41:6. [doi: 10.11604/pamj.2022.41.6.28946]
Available online at: https://www.panafrican-med-journal.com//content/article/41/6/full
Prognostic value of Epstein-Barr virus DNA load in nasopharyngeal carcinoma: a meta-analysis
Imane EL Alami1,2, ![]() Amina Gihbid1,3, Hicham Charoute1, Wafaa Khaali1, Selma Mohamed Brahim1, Nezha Tawfiq4, Rachida Cadi3, Khalid Belghmi2,
Amina Gihbid1,3, Hicham Charoute1, Wafaa Khaali1, Selma Mohamed Brahim1, Nezha Tawfiq4, Rachida Cadi3, Khalid Belghmi2, ![]() Mohammed El Mzibri5, Meriem Khyatti1,&
Mohammed El Mzibri5, Meriem Khyatti1,&
&Corresponding author
The present meta-analysis was conducted to evaluate the prognostic value of pre and post-Epstein Barr Virus (EBV) DNA load testing and to assess the clinical benefit of using this molecular approach in the prognosis for a better nasopharyngeal carcinoma (NPC) management. Relevant studies were searched in different database until May 2020. Patient´s outcomes overall survival (OS), disease free survival (DFS), progression-free survival (PFS), distant-metastasis-free survival (DMFS), and local-regional-failure-free survival (LRFS), hazard ratios (HRs) and 95% confidence intervals (CIs) were extracted from selected studies. The association of pre and post-EBV DNA load and survival outcomes was assessed using review manager and the pooled HRs with 95% CIs were calculated. Twenty-six eligible studies were included in this meta-analysis, with a total of 9966 patients. Pooled HRs showed that EBV DNA levels before and after treatment are significantly associated with survival outcomes, with HR (95% CI) of 2.09 [1.74, 2.51] for OS, 1.77 [1.19, 2.62] for DFS, 2.53 [2.18, 2.92] for DMFS, 1.78 [1.45, 2.19] for LRFS and 2.17 [1.91, 2.47] for PFS in pre-EBV DNA, and an HR (95%) of 4.52 [2.44, 8.36], 4.08 [2.38, 6.99], 5.59 [ 3.58, 8.71] and 8.88 [5.29, 14.90] for OS, DFS and PFS and DMFS in post-EBV DNA, respectively. High pre and post-EBV DNA levels were significantly associated with poor NPC patient´s survival outcomes; which clearly confirm the high interest to introduce viral EBV DNA load as a prognostic biomarker for NPC management.
Nasopharyngeal carcinoma (NPC) represents 23.8% of all head and neck cancers, making it the second most common head and neck squamous cell carcinomas (HNSCCs) after laryngeal cancers [1]. This cancer has a striking geographical distribution; the highest ethnic pattern of incidence arises from Southern Asia, especially in South China where it ranges between 15 and 50 cases per 100,000 of the population. North African countries, some countries of the Arabic peninsula, the Caribbean and the Eskimo lands in Alaska and Greenland are considered areas of intermediate incidence for NPC, with incidence ranging from 3 to 8 cases per 100,000 inhabitants [2,3]. In Morocco, the incidence of NPC in men and women is 4.2/100.000 and 1.2 /100.000, respectively (cancer registry of Casablanca, 2012). Nasopharyngeal carcinoma has a multifactorial etiology; a close association between NPC and the oncogenic pathogen Epstein-Barr virus (EBV) was largely established. Furthermore, environmental and genetic components were also involved in the development of this malignancy [3-6]. However, whatever the geographic distribution and the risk factors of NPC, management of NPC presents a real challenge. Nasopharyngeal carcinoma diagnosis is often difficult and late due to the profound location of the nasopharynx and the nonspecific nature of the clinical symptoms, causing treatment failure and high rate of mortality [4]. Globally, and due to its inherent anatomic constraints and high degree of radio-sensitivity, NPC is mainly treated with concurrent chemo-radiotherapy [5]. Unfortunately, the rate of local recurrence and distant metastasis after 5 years of the initial treatment is still high and ranges from 8.2 to 22.0%. Biomarkers for monitoring therapeutic efficacy and recurrence at follow-up time points are therefore essential for the management of NPC [6].
Currently, it´s widely accepted that EBV is the corner stone in NPC initiation, development and progression, and was therefore the central key in the development of various strategies for NPC diagnosis, follow-up and prognosis. Recent advances in molecular biology have made an outstanding contribution to our understanding of genetic and immunological pathways in NPC development highlighting some interesting biomarkers that could be used in the early diagnosis, effective prognosis and/or as therapeutic targets [7]. In this field, growing interest was given to the assessment of plasmatic EBV viral load as a biomarker for screening, diagnosis and monitoring of NPC, and reported results clearly showed that evaluation of EBV DNA loads using the quantitative PCR is highly sensitive and specific as compared to the serological tests [7,8]. Accordingly, it has been reported that high levels of cell-free EBV DNA before chemo-radiotherapy predict a poor prognosis. Moreover, a detectable cell-free EBV DNA at the end of the treatment appears to be a very good indicator of disease recurrence and distant metastasis [6]. During last decades, a great number of studies have been conducted to evaluate the use of EBV DNA load in the monitoring of NPC and consistent results convert to suggest the EBV DNA load quantification as a promising biomarker for NPC diagnosis and prognosis. However, these studies present a great heterogeneity regarding the cutoff used in the evaluation of the prognosis value of EBV DNA load, the protocol used for DNA extraction and EBV DNA quantification approach. The present study was planned to conduct a meta-analysis to evaluate the prognostic value of the EBV DNA load testing and to assess the interest of using this molecular approach in the diagnosis and prognosis of NPC for a better management of this disease.
Search strategy: the present meta-analysis was performed according to PRISMA guidelines and all studies focusing on EBV DNA quantification in NPC were discerned. Systematic search strategies were conducted via a range of online literature databases prior to May 2020, including PubMed, Embase, Google scholar and Web of Science. Peer-reviewed literature was retrieved based on the following key words in all databases: ("nasopharyngeal carcinoma" or NPC) and ("EBV DNA load" or "Epstein-Barr virus DNA" or "Epstein-Barr virus DNA load"). Additional studies not covered by the adopted search strategy, were further identified by examining the bibliographies of relevant papers. A table reporting all used papers and the databases used to extract them was added as Annex 1.
Inclusion and exclusion criteria: in this meta-analysis, all available descriptive and analytic studies satisfying at least one of the following criteria were included: i) Plasma EBV DNA load was quantified; ii) the association between different clinical outcomes of treatment (overall survival (OS), disease free survival (DFS), progression-free survival (PFS), loco-regional relapse free survival (LRFS), distant metastasis-free survival (DMFS) and EBV DNA levels was analyzed; iii) high pre-treatment EBV DNA (pre-EBV DNA)/post-treatment EBV-DNA (post-EBV DNA) versus low pre-EBV DNA/ post-EBV DNA were compared; iv) hazard ratios (HRs) and 95% confidence intervals (CIs) of outcomes were mentioned. In addition, meta-analyses, reviews, comments, conference abstracts, case reports and studies not reporting basic and informative data were excluded.
Data extraction: with respect to the inclusion criteria, available data from all included studies were extracted by two independent authors and in case of any inconsistency, a third author was consulted. The following data were retrieved from eligible studies: name of the first author, year of publication, geographical location of the study, study period, study design, number of patients and controls. Additional data regarding published results were also extracted including the median follow-up time, cutoff values of EBV DNA load, pre and post-EBV DNA levels, survival outcomes (OS, DFS, PFS, LRFS, and DMFS), statistical evaluations (HRs and 95% CIs).
Endpoints definition: the main endpoint of OS was defined as the time from random assignment until death. While survival patients were censored at the date of the last follow-up. Overall, DFS was defined as the time from randomization until disease recurrence or death from any cause. Progression-free survival corresponded to the time from randomization until tumor progression or death, whichever occurs first. Loco-regional relapse free survival was determined as the time from randomization to first loco-regional recurrence or death, while DMFS was defined as the time from randomization to the first detection of distant metastasis on imaging or death. Of note, DFS and RFS reported in some studies were used to represent DMFS and LRFS or PFS, respectively.
Statistical analysis: the present meta-analysis was performed using review manager (RevMan) (version 5.3, the Cochrane Collaboration, Oxford, England). Pooled HRs and corresponding 95% CIs were used to evaluate the association between pre and post-EBV DNA load and survival outcomes. HR>1 indicates higher risk for the occurrence of events (e.g., distant metastasis, death, relapse, progression, etc). Heterogeneity among studies was evaluated using the Q test, and the statistical significance was set to p-value<0.1. The I2 index was then used to evaluate the proportion of variation within studies. An I2 below 50% and p>0.1 indicated an absence of heterogeneity, while an I2 ranging between 50% and 100% or p<0.1 indicated a presence of heterogeneity. We also conducted a subgroup meta-analysis study to evaluate whether cutoff of pre-EBV DNA load may have affected the pooled results. To this end, studies were divided into two groups, a first group using a cutoff >1500 copies/ml and a second group using a cutoff ≤1500 copies/ml. Another subgroup analysis was carried out based on follow up duration, one group of studies with a follow up less than 3 years and the other one of studies with a follow up of more than 3 years. Furthermore, funnel plots were generated to evaluate small-study bias visually, and Begg´s test was used to examine the potential publication bias statistically. Finally, meta-regression and subgroup meta-analyses were carried out to assess the potential studies sources of heterogeneity and confounding effects.
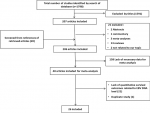
Study selection and characteristics: systematic search strategies conducted in the various online literature databases have led to an initial screening of 1798 studies. After screening of titles and abstracts, 1591 were removed. From the remaining 207 articles, 21 were excluded: 2 papers were limited to the abstracts, 1 commentary, 13 were review papers, 3 meta-analyses and 2 were not related to our topic. Moreover, 206 articles were obtained as initial database after adding 20 studies from references of retrieved articles. Following a detailed evaluation of these 206 studies with respect to adopted inclusion/exclusion criteria, 158 articles lacked necessary data, 21 lacked quantitative survival outcomes related to EBV DNA load and one found to be a duplicate article were excluded. A total of 26 relevant articles studying 9966 patients were included for the final analysis (Figure 1). Among the 26 eligible studies, 16 were retrospective and 10 prospective studies [2,8-32]. Total subjects per study varied between 34 and 1501 patients, with only 2 studies conducted on a sample size exceeding 1000 patients. The characteristics of these studies are reported in Table 1 and show that most studies were conducted in high NPC-endemic areas; 20 in China, 3 in Taiwan and 2 in Thailand. Only 1 study was performed in a low-endemic country and was conducted in patients from Netherlands. The cut-off value of pre-EBV DNA for predicting outcomes varied across studies and ranged between 0 and 10000 copies/ml; the most common employed values being 1500 and 4000 copies/ml. The median follow-up duration ranged from 25 months to 62 months.
Pre-EBV DNA levels and survival outcome: pooled analyses of the 26 selected studies showed that pre-EBV DNA presents a significant prognostic value, with HR (95% CI) of 2.09 [1.74, 2.51] for OS, 1.77 [1.19, 2.62] for DFS, 2.53 [2.18, 2.92] for DMFS, 1.78 [1.45, 2.19] for LRFS and 2.17 [1.91, 2.47] for PFS, indicating that high levels of pre-EBV DNA were significantly associated with higher risk of death, recurrence and distant metastasis in the early phases of NPC management (Table 2). Furthermore, heterogeneity test revealed a significant heterogeneity between-studies in OS, DFS and pre-EBV-DN A with I2 =48%, p=0.007 and I2=65%, p=0.04, respectively; thus, a random effect model was applied to calculate the association of pre-EBV DNA with these parameters. A fixed effect model was used for DMFS, LRFS and PFS as there was no sign of heterogeneity among the studies with I2=18%, p=0.26, I2=11%, p=0.34 and I2=0%, p=0.82 respectively (Table 2).
Post-EBV DNA levels and survival outcome: the association between post-EBV DNA and survival parameters was also assessed. A fixed-effect model was used for LRFS since there was no sign of heterogeneity among the studies (p= 0.40, I2 =0%). For the other survival outcome parameters, statistical analyses showed significant heterogeneity across the included studies for OS (I2=88%, p=0.00001), DFS (I2=72%, p=0.01), DMFS (I2=72%, p=0.0004) and PFS (I2=73%, p=0.0001), and thus random effect model was applied to calculate the association of post-EBV DNA with these parameters. Pooled results clearly showed that high post-EBV DNA load was strongly associated with risk of metastasis with an HR (95%) of 8.88 [5.29,14.90]. In fact, the risk of metastasis was 8-fold higher for patients with high post-EBV DNA levels compared with low post-EBV DNA levels. Post-EBV DNA HR (95% CI) for OS, DFS and PFS were 4.52 [ 2.44, 8.36], 4.08 [2.38, 6.99] and 5.59 [3.58, 8.71], respectively. However, a weak association between post-EBV DNA and LRFS was obtained with an HR (95%) of 1.64 [0.99 2.71] (Table 2).
Subgroup analysis based on pre-EBV DNA cutoffs: to investigate potential sources of heterogeneity within the studies, a subgroup analysis was performed based on EBV DNA load cutoff used in the included studies. Results of the subgroup analyses are reported in (Table 3). Overall, a pre-EBV DNA cutoff ≤1500 copies/ml remains the most used cutoff in the included studies. Results of pre-EBV DNA showed no significant differences in the results of subgroups analysis compared with those of the original analysis. In fact, meta-analysis of pooled results for survival parameters were not affected by the EBV DNA load cutoffs. For the studies using a pre-EBV DNA cutoff of ≤1500 copies/ml, the pooled HR (95% CI) for OS, DMFS, LRFS and PFS were 1.88 [1.56,2.26], 2.39 [1.83,3.11], 1.53 [0.84, 2.76], and 2.07 [1.80, 2.37], respectively. Moreover, for the studies using a pre-EBV DNA cutoff of >1500 copies, the pooled HR and CI for OS, DFS, DMFS, LRFS and PFS were 2.47 [1.84, 3.31], 1.77 [1.19, 2.62], 2.59 [2.17, 3.09], 1.87 [1.41,2.47], and 2.18 [1.78, 2.7], respectively. In addition, no evidence between study heterogeneity was found for pre-EBV DNA ≤1500 associated OS, DMFS and PFS and pre-EBV DNA > 1500 associated DMFS, LRFS and PFS (p<0.01). Although, a very low heterogeneity was found for pre-EBV DNA ≤1500 associated LRFS and pre-EBV DNA >1500 associated OS and DFS (p>0.1)
Subgroup analysis based on follow up duration: in the present meta-analysis, the included studies were sub-divided in two groups according to the follow up duration; the first subgroup consisted of studies with a follow up less than or equal to 3 years and the second one was studies with a follow up of more than 3 years. Pooled HRs showed that whatever the follow up duration, pre-EBV DNA levels were significantly associated with poorer OS, DFS, DMFS, LRFS and PFS (Table 4). For studies with a follow up duration ≤ to 3 years, our data showed a significant heterogeneity within 14 and 3 studies for OS and DFS parameters, respectively (p>0.01), whereas a very low heterogeneity was found for DMFS, LRFS and PFS parameters (p<0.01). For studies with a follow up duration > to 3 years, no significant heterogeneity within studies was revealed (p<0.01) (Table 4).
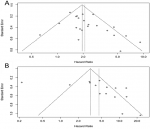
Assessment of publication bias: using Begg´s test to analyze publication bias, no evidence of bias was found in pre-EBV DNA associated DFS, DMFS, LRFS (p=0.4634, p=0.5355 and p=0.8593, respectively) and post-EBV DNA associated OS, DFS, DMFS and LRFS (p=0.08663, p=0.4811, p=0.07077 and p=0.4756, respectively) (Table 5). However, a publication bias was observed in the pre-EBV DNA OS (p= 0.03983) and PFS (p=0.006583), and post-EBV DNA PFS (p=0.04864) (Table 5). The funnel plots of the 22 included studies reporting the association between pre-EBV DNA levels and OS and of the 15 included studies that examined post-EBV DNA associated OS are reported in Figure 2.
A close association between EBV infection and the NPC was widely reported. Based on this association, several EBV derived molecules are widely used as biomarkers for NPC management. Early studies highlighted EBV serology as an important biomarker for both screening and early detection of NPC in endemic areas [33-35]. However, the main limitation of these serological tests is their poor capacity to assess therapeutic outcomes for NPC patients. Indeed, scientific evidences have shown that the levels of some antibodies remain high even in patients in complete remission [36,37]. Recently, the discovery of cell- free nucleic acids biomarkers for NPC has revolutionized the disease management. Circulating EBV DNA is one of the most non-invasive studied biomarkers of NPC and clinical usefulness for screening, diagnosis and prognosis of NPC patients in endemic areas is widely documented [36,38]. In the present meta-analysis, we evaluated the pre and post-EBV DNA load testing in order to assess this molecular approach in the prognostic management of this disease. Accordingly, the association between pre and post -EBV DNA load and patient´s outcomes (OS, PFS, DMFS, and LRFS) was performed. This meta-analysis included a total of 16 retrospective and 10 prospective studies including 9966 patients. Our results clearly showed that patients with high levels of pre-EBV DNA had higher risk of death, loco-regional recurrence and distant metastasis, compared to patients with low levels of pre-EBV DNA. Indeed, pooled HR values achieved 2.09 (95% CI=1.74, 2.51, p<0.00001) for OS, 1.77 (95% CI=1.19, 2.62, p<0.005) for DFS, 2.53 (95% CI=2.18, 2.92, p<0.00001) for DMFS, 1.78 (95% CI=1.45, 2.19, p<0.00001) for LRFS and 2.17 (95% CI=1.91, 2.47, p<0.00001) for PFS. Similarly, Weng et al. have reported that patients with low pre-EBV DNA levels had longer survival rates compared to those with high pre-EBV DNA [38]. Even though most studies included in this meta-analysis were conducted in endemic areas, studies from non-endemic and middle-endemic areas reported a similar prognostic value of pre and post-EBV DNA load. However, these studies were excluded from this meta-analysis due to the lack of HRs values or the EBV DNA load was measured in nasopharyngeal brushings or biopsies. Of particular interest, a study including a cohort of 36 Western patients with stage IIb-IVb nasopharyngeal cancer, showed that pre-EBV DNA levels monitoring can allow the detection of disease recurrence and metastases [39].
Similarly, Alfieri et al. have carried out a study on 130 locally-advanced EBER positive NPC Italian patients and revealed that DFS and OS were significantly longer in patients with negative pre-EBV DNA load (p=0.03 and p=0.02, respectively) [40]. In the same population, Alessi et al. showed that EBV DNA load was significantly associated with DFS (p=0.05) [41]. Furthermore, Mazurek et al. highlighted the important role of EBV DNA assessment in the diagnostic of NPC patients with T1-T2 tumors in Poland [42]. Another study from Russia recommended the simultaneous use of plasma EBV DNA loads and VCA/IgA antibody levels as diagnostic and monitoring markers for the undifferentiated type of NPC in non-endemic regions [43]. The measurement of EBV DNA load before and after treatment of 22 consecutive Dutch NPC patients revealed that EBV DNA in plasma became undetectable after treatment, and suggest this marker as useful one in a low NPC risk area [37]. Moreover, an American study highlighted that EBV DNA levels was more informative compared to EA serology for distinguishing remission from recurrence NPC disease [37]. In middle endemic areas; it have been reported that EBV DNA load quantification after treatment may be a good predictor of OS and PFS for Tunisian patients with NPC [44]. The persistence of EBV DNA in blood was found to be a good indicator of therapy failure of patients and most studies reported a significant correlation between EBV DNA in plasma after treatment, OS and DMFS [2,41]. Interestingly, in this meta-analysis, pooled HRs revealed that the risk of mortality and metastasis was respectively 8 and 5 fold higher for patients with high post-EBV DNA levels as compared to those with low post-EBV DNA levels. Measuring the change of EBV DNA loads before and after treatment, may be a helpful non-invasive and fast tool to attempts loco-regional and distant recurrences after chemo-radiotherapy.
Difference between these studies (including study design, sample size, ethnicity) has been widely reported and discussed. These differences could be potential sources of heterogeneity between results of studies. In this field, analysis of data from this meta-analysis also indicates a significant heterogeneity between pre and post-EBV DNA loads and most of clinical outcomes (I2>50%, p<0.1). To explore the source of this heterogeneity and possible publication bias, we have conducted subgroup analysis based on cutoff values and follow up duration. Our results of subgroups analysis show that pre-EBV DNA ≤1500 or >1500 copies/ml was significantly associated with survival outcomes. Of particular interest, no significant difference in the results of subgroups analysis compared with those of the original analysis was observed. Worldwide, the cutoff for EBV DNA load assessment is well discussed and documented. Although there is no international recommendation regarding the optimal EBV cutoff points for pre-EBV DNA, studies used commonly the cutoff values of 1500 copies/ml and 4000 copies/ml [45]. Accordingly, 10 studies from this meta-analysis used a cutoff of 1500 copies/ml and four used 4000 copies/ml as cutoff for survival analysis. Recently, Lertbutsayanukul et al. have analyzed a series of cutoffs (0, 1500, 2010, 2300, 4000 and 50000 copies/ml) and suggested 2300 copies/ml as the optimal value in terms of sensitivity and specificity for predicting 3 years OS, PFS and DMFS [46]. There´s therefore evidence that more studies are needed to establish a standardized cutoff, an optimum pre-EBV DNA cutoff values may serve as guidance for NPC disease risk stratification, combined to TNM staging or alone.
In follow up duration subgroups, significant heterogeneity was found only for the OS and DFS, and no significant heterogeneity within studies with a follow up duration superior to 3 years was observed, suggesting that duration of follow-up couldn´t be a potential source of heterogeneity, and others sources of heterogeneity should be explored. In a previous meta-analysis, the nature of samples (plasma or serum), tumor grade, cutoff values of pre-EBV DNA levels (<1500, ≥1500, <4000, and ≥4000 copies/ml) and detection time of post-EBV DNA levels (1 week, 5 or 8 weeks and 3 months after treatment) were found to be potential sources of heterogeneity [45,47]. Interestingly, another meta-analysis highlighted that detection of EBV DNA in both plasma or serum had higher sensitivity and specificity in prognosis of NPC, but EBV DNA in plasma was found to have a higher accuracy than in serum [47]. On the other hand, Zhang et al. have reported that tumor grade, cutoff value and histological differentiation influence moderately, but not significantly, the heterogeneity between studies [45]. Moreover, Qu et al. recommended to use any detection time point for post-EBV DNA measurement, whatever 1 week or 3 months after treatment [48]. Overall, we observed that the heterogeneity between studies affect poorly the sensitivity and specificity of this biomarker, and suggest that, whatever the quantification method or the cutoff used, the prognostic utility of EBV DNA load in NPC still highly performing. The present meta-analysis is very informative and highlights the impact of high EBV DNA load in NPC persistence and treatment failure. However, there are still some limitations to be considered for further investigations: i) most of the included subjects were Asiatic patients, neglecting the ethnic and genetic varieties that can influence the expression levels of the EBV DNA loads; ii) patient management, from diagnosis to the end of follow-up, could be largely diverse between the different medical centers, which may influence the pooled results; iii) the association between DFS and pre-EBV DNA ≤1500 wasn´t assessed because of the lack of studies.
This meta-analysis demonstrated that pre-EBV DNA load can predict patient prognosis at the early step of NPC management. Moreover, post-EBV DNA levels can be an effective tool for detection of recurrence or metastasis in post-treatment surveillance, besides imaging exams (MRI, TEP-CT).
Funding: the present research project was funded by Cancer Research Institute (IRC). Ref:201932.
What is known about this topic
- Most of the patients with Nasopharyngeal carcinoma have poor prognostic;
- Plasmatic EBV viral load was suggested as a molecular biomarker for NPC diagnosis and monitoring.
What this study adds
- The present meta-analysis summarized data of a total of 16 retrospective and 10 prospective studies including 9966 patients;
- Patients with high levels of pre-EBV DNA had higher risk of death, loco-regional recurrence and distant metastasis, compared to patients with low levels of pre-EBV DNA;
- The risk of mortality and metastasis was respectively 8 and 5 fold higher for patients with high post-EBV DNA levels as compared to those with low post-EBV DNA levels; high pre-EBV DNA load and detectable post-EBV DNA load is associated with NPC persistence and treatment failure.
The authors declares no competing interests.
Study concepts: Meriem Khyatti, Nezha Tawfiq and Mohammed El Mzibri; study design: Meriem Khyatti, Amina Gihbid and Imane EL Alami; data acquisition: Imane EL Alami, Amina Gihbid and Salma Mohamed Brahim; quality control of data and algorithms: Imane El Alami, Amina Gihbid and Wafaa Khaali; data analysis and interpretation: Hicham Charoute, Imane El Alami and Amina Gihbid; statistical analysis: Hicham Charoute, Imane El Alami and Amina Gihbid; manuscript preparation: Amina Gihbid, Imane El Alami, Wafaa Khaali and Khalid Belghmi; manuscript editing: Mohammed El Mzibri and Meriem Khyatti; manuscript review: Nezha Tawfiq, Rachida Cadi, Mohammed El Mzibri and Meriem Khyatti. All the authors have read and agreed to the final manuscript.
Table 1: global characteristics of eligible studies selected for the meta-analysis
Table 2: association between pre/post-EBV DNA and survival outcomes
Table 3: association between pre-EBV DNA cutoffs and survival outcomes
Table 4: distribution of outcomes parameters according to the follow up duration
Table 5: evaluation of publication bias
Figure 1: flow diagram of study selection
Figure 2: A) the funnel plot of the 22 included studies that reported the association between pre-EBV DNA levels and OS; B) the funnel plot of the 15 included studies that examined post-EBV DNA associated OS
Annex 1: list of papers used in the meta-analysis and the databases used for their extraction (PDF-336kb)
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018 Nov;68(6):394-424. PubMed | Google Scholar
- Lin J-C, Wang WY, Chen KY, Wei YH, Liang WM, Jan JS et al. Quantification of plasma Epstein-Barr Virus DNA in patients with dvanced nasopharyngeal carcinoma. N Engl J Med. 2004 Jun 10;350(24):2461-70. PubMed | Google Scholar
- Ji MF, Huang QH, Yu X, Liu Z, Li X, Zhang LF et al. Evaluation of plasma Epstein-Barr virus DNA load to distinguish nasopharyngeal carcinoma patients from healthy high-risk populations in Southern China. Cancer. 2014 May 1;120(9):1353-60. PubMed | Google Scholar
- Adham M, Greijer AE, Verkuijlen SAWM, Juwana H, Fleig S, Rachmadi L et al. Epstein-Barr Virus DNA load in nasopharyngeal brushings and whole blood in nasopharyngeal carcinoma patients before and after treatment. Clin Cancer Res. 2013 Apr 15;19(8):2175-86. PubMed | Google Scholar
- Ma B, Hui E, Chan A. Systemic approach to improving treatment outcome in nasopharyngeal carcinoma: current and future directions. Cancer Sci. 2008 Jul;99(7):1311-8. PubMed | Google Scholar
- Chen Y-H, Chang KP, Chu SC, Yen TC, Wang LY, Chang JTC et al. Value of early evaluation of treatment response using 18F-FDG PET/CT parameters and the Epstein-Barr virus DNA load for prediction of outcome in patients with primary nasopharyngeal carcinoma. Eur J Nucl Med Mol Imaging. 2019 Mar;46(3):650-660. PubMed | Google Scholar
- Peng H, Guo R, Chen L, Zhang Y, Li WF, Mao YP et al. Prognostic impact of plasma Epstein-Barr Virus DNA in patients with nasopharyngeal carcinoma treated using intensity-modulated radiation therapy. Sci Rep. 2016 Feb 29;6:22000. PubMed | Google Scholar
- Chen WH, Tang LQ, Guo SS, Chen QY, Zhang L, Liu LT et al. Prognostic value of plasma Epstein-Barr Virus DNA for local and regionally advanced nasopharyngeal carcinoma treated with cisplatin-based concurrent chemoradiotherapy in intensity-modulated radiotherapy era. Medicine (Baltimore). 2016 Feb;95(5):e2642. PubMed | Google Scholar
- Lan M, Chen C, Huang Y, Mao M, Han F, Liao J et al. Elevated plasma fibrinogen level shows superior prognostic value than Epstein-Barr virus DNA load for stage IVA/B nasopharyngeal carcinoma patients in the intensity-modulated radiotherapy era. Oncotarget. 2016 Jul 19;7(29):46242-46252. PubMed | Google Scholar
- Peng H, Guo R, Chen L, Zhang Y, Li WF, Mao YP et al. Prognostic impact of plasma Epstein-Barr Virus DNA in patients with nasopharyngeal carcinoma treated using intensity-modulated radiation therapy. Sci Rep. 2016 Feb 29;6:22000. PubMed | Google Scholar
- Jin YN, Yao JJ, Zhang F, Wang SY, Zhang WJ, Zhou GQ et al. Is pretreatment Epstein-Barr virus DNA still associated with 6-year survival outcomes in locoregionally advanced nasopharyngeal carcinoma? J Cancer. 2017 Mar 12;8(6):976-982. PubMed | Google Scholar
- Stoker SD, Wildeman MA, Novalic Z, Fles R, van der Noort V, de Bree R et al. Can Epstein-Barr virus DNA load in nasopharyngeal brushings or whole blood predict recurrent nasopharyngeal carcinoma in a non-endemic region? A prospective nationwide study of the Dutch Head and Neck Oncology Cooperative Group. Eur Arch Otorhinolaryngol. 2016 Jun;273(6):1557-67. PubMed | Google Scholar
- Xu T, Huang Z, Deng Y, Wang S, Su B, Wei W et al. Clinical implications of hepatitis B viral infection in Epstein-Barr virus-associated nasopharyngeal carcinoma. J Clin Virol. 2015 Mar;64:64-71. PubMed | Google Scholar
- Wang WY, Twu CW, Chen HH, Jiang RS, Wu CT, Liang KL et al. Long-term survival analysis of nasopharyngeal carcinoma by plasma Epstein-Barr virus DNA levels. Cancer. 2013 Mar 1;119(5):963-70. PubMed | Google Scholar
- Xu T, Huang Z, Su B, Wang S, Wang D, Wang C et al. Prognostic significance of circulating CD19+ B lymphocytes in EBV-associated nasopharyngeal carcinoma. Med Oncol. 2014 Oct;31(10):198. PubMed | Google Scholar
- Lv JW, Chen YP, Zhou GQ, Tang LL, Mao YP, Li WF et al. Cigarette smoking complements the prognostic value of baseline plasma Epstein-Barr virus deoxyribonucleic acid in patients with nasopharyngeal carcinoma undergoing intensity-modulated radiation therapy: a large-scale retrospective cohort study. Oncotarget . 2016 Mar 29;7(13):16806-17. PubMed | Google Scholar
- Wang WY, Lin TY, Twu CW, Tsou HH, Lin PJ, Liu YC et al. Long-term clinical outcome in nasopharyngeal carcinoma patients with post-radiation persistently detectable plasma EBV DNA. Oncotarget. 2016 Jul 5;7(27):42608-42616. PubMed | Google Scholar
- Zhao FP, Liu X, Chen XM, Lu J, Yu BL, Tian WD et al. Levels of plasma Epstein-Barr virus DNA prior and subsequent to treatment predicts the prognosis of nasopharyngeal carcinoma. Oncol Lett. 2015 Nov;10(5):2888-2894. PubMed | Google Scholar
- Shen T, Tang LQ, Luo DH, Chen QY, Li PJ, Mai DM et al. Different prognostic values of plasma Epstein-Barr Virus DNA and maximal standardized uptake value of 18F-FDG PET/CT for nasopharyngeal carcinoma patients with recurrence. PLoS One. 2015 Apr 8;10(4):e0122756. PubMed | Google Scholar
- Wei W, Huang Z, Li S, Chen H, Zhang G, Li S et al. Pretreatment Epstein-Barr Virus DNA load and cumulative cisplatin dose intensity affect long-term outcome of nasopharyngeal carcinoma treated with concurrent chemotherapy: experience of an institute in an endemic Area. Oncol Res Treat. 2014;37(3):88-95. PubMed | Google Scholar
- Leung SF, Chan KCA, Ma BB, Hui EP, Mo F, Chow KCK et al. Plasma Epstein-Barr viral DNA load at midpoint of radiotherapy course predicts outcome in advanced-stage nasopharyngeal carcinoma. Ann Oncol. 2014 Jun;25(6):1204-8. PubMed | Google Scholar
- Twu CW, Wang WY, Liang WM, Jan JS, Jiang RS, Chao J et al. Comparison of the prognostic impact of serum anti-EBV antibody and plasma EBV DNA assays in nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2007 Jan 1;67(1):130-7. 2007;67(1):130-137. PubMed | Google Scholar
- Chan ATC. Plasma Epstein-Barr Virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinoma. J Natl Cancer Inst. 2002 Nov 6;94(21):1614-9 PubMed | Google Scholar
- Zhang Y, Li WF, Mao YP, Guo R, Tang LL, Peng H et al. Risk stratification based on change in plasma Epstein-Barr virus DNA load after treatment in nasopharyngeal carcinoma. Oncotarget. 2016 Feb 23;7(8):9576-85. PubMed | Google Scholar
- Wang HM, Lin TL, Kuo YC, Li HP, Chang KP, Lin CY et al. Correlation between overall survival and differential plasma and tissue tumor marker expression in nasopharyngeal carcinoma patients with different sites of organ metastasis. Oncotarget. 2016 Aug 16;7(33):53217-53229. PubMed | Google Scholar
- Prayongrat A, Chakkabat C, Kannarunimit D, Hansasuta P, Lertbutsayanukul C. Prevalence and significance of plasma Epstein-Barr Virus DNA level in nasopharyngeal carcinoma. J Radiat Res. 2017 Jul 1;58(4):509-516. PubMed | Google Scholar
- JHsu CL, Chang KP, Lin CY, Chang HK, Wang CH, Lin TL et al. Plasma Epstein-Barr virus DNA concentration and clearance rate as novel prognostic factors for metastatic nasopharyngeal carcinoma. Head Neck. 2012 Aug;34(8):1064-70. PubMed | Google Scholar
- Wang WY, Twu CW, Chen HH, Jan JS, Jiang RS, Chao JYC et al. Plasma EBV DNA clearance rate as a novel prognostic rarker for metastatic/recurrent nasopharyngeal carcinoma. Clin Cancer Res. 2010;16(3):1016-1024. PubMed | Google Scholar
- Huang CL, Sun ZQ, Guo R, Liu X, Mao YP, Peng H et al. Plasma Epstein-Barr Virus DNA load after induction chemotherapy predicts outcome in locoregionally advanced nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2019;104(2):355-361. PubMed | Google Scholar
- Chen QY, Tang QN, Tang LQ, Chen WH, Guo SS, Liu LT et al. Pretreatment serum amyloid A and C-reactive protein comparing with Epstein-Barr Virus DNA as prognostic indicators in patients with nasopharyngeal carcinoma: a prospective study. Cancer Med. 2019 Aug;8(10):4633-4643. PubMed | Google Scholar
- Liu M, Fang S, Huang W, Wang H, Tian Y, Huang R et al. Clinical characteristics and prognostic value of pre‐retreatment plasma epstein‐barr virus DNA in locoregional recurrent nasopharyngeal carcinoma. Cancer Med. 2019;8(10):4633-4643. PubMed | Google Scholar
- Lertbutsayanukul C, Kannarunimit D, Prayongrat A, Chakkabat C, Kitpanit S, Hansasuta P. Prognostic value of plasma EBV DNA for nasopharyngeal cancer patients during treatment with intensity-modulated radiation therapy and concurrent chemotherapy. Radiology and Oncology. 2018;52(2):195-203. PubMed | Google Scholar
- Tay JK, Chan SH, Lim CM, Siow CH, Goh HL, Loh KS. The role of Epstein-Barr Virus DNA load and serology as screening tools for nasopharyngeal carcinoma. Otolaryngol Head Neck Surg. 2016 Aug;155(2):274-80. PubMed | Google Scholar
- Chen Y, Xin X, Cui Z, Zheng Y, Guo J, Chen Y et al. Diagnostic value of serum Epstein-Barr Virus capsid antigen-IgA for nasopharyngeal carcinoma: a meta-analysis based on 21 studies. Clin Lab. 2016;62(6):1155-66. PubMed | Google Scholar
- Cai YL, Li J, Lu AY, Zheng YM, Zhong WM, Wang W et al. Diagnostic significance of combined detection of Epstein-Barr virus antibodies, VCA/IgA, EA/IgA, Rta/IgG and EBNA1/IgA for nasopharyngeal carcinoma. Asian Pac J Cancer Prev. 2014;15(5):2001-6. PubMed | Google Scholar
- Fan H, Nicholls J, Chua D, Chan KH, Sham J, Lee S et al. Laboratory markers of tumor burden in nasopharyngeal carcinoma: a comparison of viral load and serologic tests for Epstein-Barr virus. Int J Cancer. 2004 Dec 20;112(6):1036-41. PubMed | Google Scholar
- Kalpoe JS, Dekker PBD, van Krieken JHJM, Baatenburg de Jong RJ, Kroes ACM. Role of Epstein-Barr virus DNA measurement in plasma in the clinical management of nasopharyngeal carcinoma in a low risk area. J Clin Pathol. 2006 May;59(5):537-41. PubMed | Google Scholar
- Weng J, Wei J, Si J, Qin Y, Li M, Liu F et al. Clinical outcomes of residual or recurrent nasopharyngeal carcinoma treated with endoscopic nasopharyngectomy plus chemoradiotherapy or with chemoradiotherapy alone: a retrospective study. PeerJ. 2017;5:e3912. PubMed | Google Scholar
- Ferrari D, Codecà C, Bertuzzi C, Broggio F, Crepaldi F, Luciani A et al. Role of plasma EBV DNA levels in predicting recurrence of nasopharyngeal carcinoma in a western population. BMC Cancer. 2012 May 30;12:208. PubMed | Google Scholar
- Alfieri S, Iacovelli NA, Marceglia S, Lasorsa I, Resteghini C, Taverna F et al. Circulating pre-treatment Epstein-Barr virus DNA as prognostic factor in locally-advanced nasopharyngeal cancer in a non-endemic area. Oncotarget. 2017 Jul 18;8(29):47780-47789. PubMed | Google Scholar
- Alessi A, Lorenzoni A, Cavallo A, Padovano B, Iacovelli NA, Bossi P et al. Role of pretreatment 18F-FDG PET/CT parameters in predicting outcome of non-endemic EBV DNA-related nasopharyngeal cancer (NPC) patients treated with IMRT and chemotherapy. Radiol Med. 2019 May;124(5):414-421. PubMed | Google Scholar
- Mazurek AM, Wygoda A, Rutkowski T, Olbryt M, Pietrowska M, Celejewska A et al. Prognostic significance of Epstein-Barr virus viral load in patients with T1-T2 nasopharyngeal cancer. J Med Virol. 2020 Mar;92(3):348-355. PubMed | Google Scholar
- Gurtsevitch VE, Senyuta NB, Ignatova AV, Lomaya MV, Kondratova VN, Pavlovskaya AI et al. Epstein-Barr virus biomarkers for nasopharyngeal carcinoma in non-endemic regions. J Gen Virol. 2017 Aug;98(8):2118-2127. PubMed | Google Scholar
- Hassen E, Farhat K, Gabbouj S, Bouaouina N, Abdelaziz H, Chouchane L. Epstein-Barr virus DNA quantification and follow-up in Tunisian nasopharyngeal carcinoma patients. Biomarkers. 2011 May;16(3):274-80. PubMed | Google Scholar
- Zhang J, Shu C, Song Y, Li Q, Huang J, Ma X. Epstein-Barr virus DNA level as a novel prognostic factor in nasopharyngeal carcinoma: a meta-analysis. Medicine (Baltimore). 2016 Oct;95(40):e5130. PubMed | Google Scholar
- Lertbutsayanukul C, Kannarunimit D, Netsawang B, Kitpanit S, Chakkabat C, Hansasuta P et al. Optimal plasma pretreatment EBV DNA cut-off point for nasopharyngeal cancer patients treated with intensity modulated radiation therapy. Jpn J Clin Oncol. 2018;48(5):467-475. PubMed| Google Scholar
- Han BL, Xu XY, Zhang CZ, Wu JJ, Han CF, Wang H et al. Systematic review on Epstein-Barr virus (EBV) DNA in diagnosis of nasopharyngeal carcinoma in Asian populations. Asian Pac J Cancer Prev. 2012;13(6):2577-2581. PubMed | Google Scholar
- Qu H, Huang Y, Zhao S, Zhou Y, Lv W. Prognostic value of Epstein-Barr virus DNA level for nasopharyngeal carcinoma: a meta-analysis of 8128 cases. Eur Arch Otorhinolaryngol. 2020 Jan;277(1):9-18. PubMed | Google Scholar