Socio-demographic characteristics and pre-hospital care of children with circulatory failure in a children's emergency room in southern Nigeria
Moses Temidayo Abiodun, Wilson Ehidiamen Sadoh
Corresponding author: Moses Temidayo Abiodun, Department of Child Health, University of Benin Teaching Hospital, Benin City, Edo State, Nigeria 
Received: 24 May 2021 - Accepted: 20 Aug 2021 - Published: 28 Sep 2021
Domain: Pediatric cardiology, Pediatrics (general)
Keywords: Circulatory failure, socio-demographic, prehospital care
©Moses Temidayo Abiodun et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Moses Temidayo Abiodun et al. Socio-demographic characteristics and pre-hospital care of children with circulatory failure in a children's emergency room in southern Nigeria. Pan African Medical Journal. 2021;40:65. [doi: 10.11604/pamj.2021.40.65.30003]
Available online at: https://www.panafrican-med-journal.com//content/article/40/65/full
Research 
Socio-demographic characteristics and pre-hospital care of children with circulatory failure in a children's emergency room in southern Nigeria
Socio-demographic characteristics and pre-hospital care of children with circulatory failure in a children´s emergency room in southern Nigeria
&Corresponding author
Introduction: circulatory failure is a major childhood emergency. Several disease-related and patient-related factors can predispose children to shock. Early detection of such factors will improve its prevention, management and outcome. This study aimed to evaluate the incidence, socio-demographic characteristics and pre-hospital care of children presenting with circulatory failure (shock) in children´s emergency room (CHER).
Methods: this study adopted cross-sectional design in CHER of the University of Benin Teaching Hospital, Nigeria, from October 2018 to March 2019. Data were collected using a semi-structured questionnaire eliciting demography, socio-economic status, pre-hospital care and presence of shock. In a sub-analysis, multiple logistic regression identified variables that are independently associated with circulatory failure in the participants, using adjusted odds ratio (OR) and 95% confidence intervals (CI).
Results: a total of 554 acutely-ill children participated in the study. Their median age was 60 (IQR: 24-132) months. Shock was present in 79 (14.3%) of the children on arrival at CHER. Children referred from private clinics were more likely to arrive CHER in shock compared to those coming directly from home (OR = 2.67, 95%CI: 1.07-6.69; p = 0.036) while children from lower socio-economic class families presented more frequently with shock than those from higher class (OR = 14.39, 95% CI: 2.61-79.44; p = 0.002). Also, children that received oral rehydration solution as pre-hospital care seemed more likely to present with shock in CHER (OR = 6.63, 95% CI: 2.15-20.46; p =0.001).
Conclusion: quality of pre-hospital care and parental socio-economic status influence the presence of shock in children seen at the emergency unit. Focused health education and prevention of finance-related delays in emergency care are needed.
Circulatory failure or shock is a common emergent morbidity encountered in acutely-ill children in the emergency room. It is a state of acute energy failure at the cellular level due to inadequate glucose and substrate delivery, hypoxemia or mitochondrial failure [1,2]. In a prospective study by Carcillo et al. [3], shock was present in 37% of children transferred to 5 regional hospitals for tertiary care. Also, shock can develop in a child while on admission. Fisher et al. [4] reported that clinical signs of shock developed in the emergency department (ED) after initially presenting without clinical signs of shock in 14% of cases in their series. Shock constitutes a life threatening illness in a child. The resultant anaerobic respiration leads to elevated serum lactate which is a poor prognostic factor in severe illness [5,6]. When shock is not recognized and reversed promptly, it leads to widespread ischaemic damage in all organ systems in the body, including the gastrointestinal system where there can be translocation of bacteria into the blood stream, contributing to systemic inflammatory response syndrome (SIRS), irreversible shock and multi-organ dysfunction syndrome (MODS) in affected children [7,8].
There are several disease-related and patient-related factors that can predispose children to circulatory failure [9,10]. Prompt recognition of these characteristics can facilitate case-specific evaluation and treatment of at-risk children. Although children have a high total body water, they are predisposed to shock because of their relatively increased basal metabolic rate and insensible water loss as well as low renal concentrating ability [11]. Also, chronic illnesses, hypothermia and malnutrition worsen severity of shock leading to presentation in emergency units in moribund conditions [12]. In addition, caregiver-related factors can influence the incidence and outcome of circulatory shock. Low parental educational and socio-economic status leads to poor health-seeking behavior which contributes to the high mortality rates in childhood emergencies in Nigeria and many sub-Saharan African countries [13,14]. Likewise, home remedies like herbal concoction with potential severe adverse reactions can contribute to deranged homeostasis and shock in children [15,16]. Hence, some baseline patient characteristics alongside potentially-modifiable factors contribute to the occurrence and prognosis of circulatory failure in acutely ill children. Considering the foregoing, the burden of circulatory failure in a practice setting can be reduced if the predisposing factors are identified and prevented in at-risk children. We hypothesized that some socio-demographic characteristics are associated with circulatory failure in acutely-ill children seen in our emergency room. Also, we aimed to identify the incidence, pre-hospital therapies and practices that predispose to shock in the setting.
Study design and setting: this study used a descriptive, cross-sectional design. It was undertaken in the Children Emergency Rooms (CHER) of the University of Benin Teaching Hospital (UBTH), in southern Nigeria, from October 2018 to March 2019.
Participants: these were children who participated in a larger study evaluating treatment and outcome of shock in CHER at the centre. They were aged 1 month to 18 years and were admitted into CHER with critical illnesses based on the inclusion criterion.
Inclusion criteria: all children aged between 1 month and 18 years with signs/ symptoms of critical illness, and whose parents consent to the study. Critical illness was defined as the presence of any acute life-threatening disorder in the child requiring urgent interventions to prevent death [17].
Exclusion criteria: all children less than 1 month old who are admitted directly into the neonatal intensive care unit. Also, children who do not meet the standard clinical definition for critical illness during the study period were excluded.
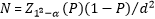
Sample size determination: the minimum sample size (N) was calculated using the qualitative variable formula for cross-sectional study [18]:
Sampling strategy: all children admitted into CHER with features of critical illnesses based on the inclusion criterion were purposively selected; they were recruited into the study if their parents or caregivers consented. This was a total population study of all eligible children during the study period.
Data collection:data were collected using a semi-structured researcher-administered questionnaire eliciting descriptive variables (demography, socio-economic status, prehospital care) and the presence of circulatory failure in the participants. Their socio-economic classification was based on their parental educational levels and occupations [19]. Blood pressure measurements was done using standard procedures with Mercury sphygmomanometer and appropriate cuffs [20]. Circulatory failure was defined based on WHO criteria (cold extremities, prolonged capillary refill >3 seconds, and fast and weak pulse) or the presence of hypotension (systolic BP < 70mmHg in infants or <70 +2n, where n = age in years for under-ten children) [11,17].
Statistical analysis: data was analysed using descriptive and inferential statistics. Categorical variables were described using frequencies and percentages while continuous variables such as age, duration of illness were described using means and standard deviations. The incidence of circulatory failure was computed based on the proportion of the participants affected at presentation. Bivariate analysis (Pearson chi-square; Mann-Whitney U test) was done to detect any significant association between the descriptive variables and circulatory failure. Variables (source of patient, maternal educational level, social class and prehospital care) that were significant (p<0.05) on binary analysis were then subjected to multivariate logistic regression to identify those that are independently associated with circulatory failure in the participants, using adjusted odds ratio (aOR) and 95% confidence intervals (CI). The level of significance was set at p < 0.05. The data analysis was carried out using the IBM Statistical Package for Social Sciences (SPSS) version 26.0 for windows.
Ethical consideration: Ethical clearance was obtained from the Research and Ethics Committee of the College of Medical Sciences, University of Benin (REC Approval Number: CMS/REC/2018/020). Permission of the Unit Head CHER was sought and informed consent was obtained from the parents/guardians of the children.
Baseline characteristics of all study participants: a total of 554 acutely-ill children took part in the study. They had a median age of 60 (IQR: 24-132) months, mean weight 16.3 ±13.6 kg, mean height 90.8 ± 33.2 cm and their female to male ratio was 1:1.2. Over a half (53.8%) of the caregivers (mothers) had secondary level of education while 42.2% and 34.6% of the families were in lower and middle socioeconomic classes respectively. Most of the children 363 (80.0%) presented to the emergency room coming directly from home; the rest of them were referred equally from both private and public hospitals. Shock was present in 79 (14.3%) of the children on arrival at CHER. Their median (IQR) duration of illness before admission was 4 (2-7) days and the pre-hospital care received included administration of ORS (7.4%) and herbal concoction (2.2%); further details are shown on Table 1.
Comparison of characteristics between the children with and without circulatory failure: comparison of characteristics between the acutely-ill children with and without cardiovascular shock showed that their sources of referral were significantly different (p = 0.011); likewise, there was significant difference between their maternal level of education (p = 0.001), pre-hospital care (p <0.001) and socio-economic classes (p < 0.001). None of the mothers who gave information on their educational level had tertiary education. The median age of children with shock was similar to that of their unaffected counterparts, 66 (24-132) vs. 60 (24-120) months respectively (p = 0.824). Also, there was no gender predilection for shock (p= 0.701) and the durations of their illnesses before admission were similar 4 (2-7) vs. 4 (2-7) days (p = 0.552). Further comparative data are shown on Table 2 below.
Multivariate logistic regression analysis for circulatory failure by selected clinical-demographic characteristics: Table 3 shows multivariate logistic regression for cardiovascular shock by selected variables; children referred from private clinics were at least two times more likely to arrive CHER in shock compared to those coming directly from home (OR = 2.67, 95% CI: 1.07-6.69; p = 0.036). Children that received ORS as pre-hospital care were significantly more likely to present in shock in CHER (OR = 6.63, 95% CI: 2.15-20.46; p = 0.001). Children from lower socio-economic class families presented more frequently with shock than those from higher class (OR = 14.39, 95% CI: 2.61-79.44; p = 0.002). Maternal level of education and child´s duration of illness were not independent risk factors of cardiovascular shock in the participants, p > 0.05.
This study shows some baseline characteristics of children presenting with circulatory failure in the emergency room; they had lower maternal levels of education than others without circulatory failure, consistent with prior reports of delayed treatment of ill children among less educated parents [13,14]. Maternal education apparently aids earlier recognition of worsening illnesses in children which can enhance prompt presentation to health facilities. Also, education can improve maternal decision-making and finance ensuring prompt access to paediatric emergency services in fee-paying health facilities [21,22]. Nevertheless, Abdulkadir et al. [23] in north-central Nigeria found that mothers´ secondary level of education was associated with late presentation of children to their emergency unit, perhaps related to their use of other community-based treatment options in the setting. In our study, children from high socioeconomic class (SEC) were less likely to present in circulatory failure in the emergency room, apparently due to their improved finance and health knowledge, consistent with earlier reports of good health-seeking behavior among families upper wealth quartiles [22,23]. However, there was no definite association between the age of the participants and the presence of shock, neonates being excluded from our study; neonatal infants are particularly vulnerable to shock because of their relatively high body surface area, insensible water loss and immature kidneys [11,21]. In contrast, Vekaria-Hirani et al. [10] in Kenya found that septic shock was commoner in the younger age groups with infants having the highest case fatality rates, apparently due to a majority of their participants being infants, including neonates. Moreover, the duration of the illnesses before admission in CHER as well as gender was not significantly associated with shock in this study; this may be due to the overall shortness of disease duration among our participants. Nonetheless, Oluwafemi et al. [12] and Isezuo et al. [24] in southern and northern Nigeria respectively found that late presentation to emergency units was associated with complications and poor outcomes among acutely-ill children.
The quality of care and referral threshold of referring hospitals as well as the expertise of transport team can influence the severity of illness at presentation in a tertiary centre [10,25]. In this index study, the source of referral was significantly associated with the presence of shock at presentation; children arriving from private clinic were twice more likely to present with circulatory failure in CHER. This could be a reflection of the severity of their illnesses before presenting at the referring clinic. Also, undue delays in transferring to a higher level of care may be present, especially when there are financial constraints, necessitated by out-of-pocket payment for healthcare. This is similar to findings by Royal et al. [26] in South Africa that critically-ill children transferred to tertiary care were unstable at arrival, possibly resulting from sub-optimal in-transit care, transport delays or illness progression. This highlights the need for efficient transport and retrieval services in our setting, comparable to those obtainable in developed countries, ensuring optimal stabilization of patients during transfer [25,27].
Furthermore, quality of prehospital care can affect the severity and outcome of childhood illnesses. Although some alternative medicines can have significant adverse effects on children, use of herbal therapies is common in African countries [15,16]. Nearly one third of our participants received pre-hospital care, and 2.2% of them took herbal concoctions before presentation in CHER. Likewise, in North-central Nigeria, Adeboye et al. [28] reported the use of several forms of traditional applications in 11.4% of paediatric emergencies and a majority of the caregivers believed that such applications cannot be used with conventional medicine, promoting late presentation to health facilities. Surprisingly, our participants who received oral rehydration salts (ORS) as prehospital care were more likely to present with shock in CHER, perhaps related to other levels of delays in accessing healthcare as well as presence of shock before the commencement of ORS. Also, wrongly prepared ORS can predispose to hyponatriemic or hypernatriemic dehydration and shock [29]. Hence, this finding should not be interpreted to undermine the usefulness of ORS in preventing dehydration in children. There is a need for regular education of caregivers on correct ORS preparation and adequate rehydration of children. The strengths of this study include its large sample size ensuring adequate power and the inclusion of all eligible children during the study period as well as the similar median ages and durations of illness (between children with and without shock) enabling subgroup comparison. Nonetheless, we acknowledge the limitation of cross-sectional study design adopted in this study, being unable to establish causal relationship. A cohort study design would have been able to compute the relative risk of circulatory failure associated with various pre-hospital therapies. Also, caregivers may not accurately recall all treatment history before presentation in the emergency setting, allowing unidentified confounders to limit the generaliseability of our findings.
Potentially modifiable factors including quality of prehospital care, maternal educational level and parental socio-economic class influence the presence of shock in children seen in emergency departments. There is a need to develop appropriate pre-hospital care services and strengthen our limited retrieval/ emergency medical services. Also, expanding the national health insurance scheme coverage to include all households in low wealth quintiles is desirable, minimizing finance-related delays in accessing healthcare.
What is known about this topic
- Several disease-related factors predispose children to circulatory failure;
- Low parental educational level leads to poor health-seeking behavior in many sub-Saharan African countries.
What this study adds
- Lower parental socio-economic class is associated with circulatory failure in children seen at CHER in the setting;
- Prior treatment in a private clinic is associated with the presence of circulatory failure on admission at the tertiary centre;
- Pre-hospital care with oral rehydration salts is not protective against circulatory failure in critically-ill children in the setting.
The authors declare no competing interests.
Wilson Ehidiamen Sadoh conceived the study; both authors designed the study; Moses Temidayo Abiodun carried out data collection and wrote the initial daft of the manuscript. Both authors were involved in data management, review and approval of the final manuscript. All the authors have read and agreed to the final manuscript.
The authors thank Benjamin Nandom (paediatric registrar) and Seun Adeola (research assistant) who participated in data collection and Enosakhare Okungbowa (biostatistician/ lecturer).
Table 1: baseline characteristics of study participants, recruited from the Children Emergency Room of the University of Benin Teaching Hospital (Nigeria), from October 2018 to March 2019 (N=554)
Table 2: comparison of characteristics between the participants with and without circulatory failure, recruited from the Children Emergency Room of the University of Benin Teaching Hospital (Nigeria), from October 2018 to March 2019 (N=554)
Table 3: multivariate logistic regression analysis for circulatory failure by selected clinical-demographic characteristics of participants, recruited from the Children Emergency Room of the University of Benin Teaching Hospital (Nigeria), from October 2018 to March 2019 (N=554)
- McLean B, Zimmerman JL. Recognition and assessment of the seriously ill patient in; fundamental Critical Care Support. Society of Critical Care Medicine. 2007;1-10.
- Pasman EA. Shock in Pediatrics Medscape. Accessed January 20, 2021.
- Carcillo JA, Kuch BA, Han YY, Day S, Greenwald BM, McCloskey KA et al. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009 Aug;124(2):500-8. PubMed | Google Scholar
- Fisher JD, Nelson DG, Beyersdorf H, Satkowiak LJ. Clinical spectrum of shock in the Pediatric Emergency Department. Pediatr Emerg Care . 2010 Sep;26(9):622-5. PubMed | Google Scholar
- Bai Z, Zhu X, Li M, Hua J, Li Y, Pan J et al. Effectiveness of predicting in-hospital mortality in critically ill children by assessing blood lactate levels at admission. BMC Pediatr. 2014 Mar 28;14:83. PubMed | Google Scholar
- Tobias AZ, Guyette FX, Seymour CW, Suffoletto BP, Martin-Gill C, Quintero J et al. Pre-resuscitation lactate and hospital mortality in prehospital patients. Prehosp Emerg Care. Jul-Sep 2014;18(3):321-7 PubMed | Google Scholar
- Hillman K. Critical care without walls. Curr Opin Crit Care. 2002 Dec;8(6):594-9. PubMed | Google Scholar
- Chen P, Billiar T. Gut microbiota and multiple organ dysfunction syndrome (MODS). Adv Exp Med Biol. 2020;1238:195-202. PubMed | Google Scholar
- Prout A, Talisa V, Mayr F, Yende, S. Pediatric sepsis and septic shock: risk factors and comorbid conditions. critical care medicine. 2016;44(12):409. Google Scholar
- Vekaria-Hirani V, Kumar R, Musoke RN, Wafula EM, Chipkophe IN. Prevalence and management of septic shock among children admitted at the Kenyatta National Hospital, longitudinal survey. Int J Pediatr. 2019 Dec 17;2019:1502963. PubMed | Google Scholar
- McKiernan CA, Lieberman SA. Circulatory shock in children: an overview. Pediatr Rev. 2005 Dec;26(12):451-60. PubMed | Google Scholar
- Oluwafemi R O, Abiodun M T. Morbidity and mortality pattern at the Emergency Paediatric Unit of mother and child Hospital Akure, Nigeria. Ann biomedical sciences. 2016 jan;15(1):151-159. Google Scholar
- Owoyemi AJ, Ladi-Akinyemi TW. Health-seeking behaviour for infants by caregivers in a semi-urban area of Lagos State, Nigeria. Niger J Health Sci. 2017 jan;17:14-9. Google Scholar
- Adedokun ST, Yaya S. Factors influencing mothers´ health care seeking behaviour for their children: evidence from 31 countries in sub-Saharan Africa. BMC Health Serv Res. BMC Health Serv Res. 2020 Sep 7;20(1):842. PubMed | Google Scholar
- Moro PA, Flacco V, Cassetti F, Clementi V, Colombo ML, Chiesa GM, et al. Hypovolemic shock due to severe gastrointestinal bleeding in a child taking an herbal syrup. Ann Ist Super Sanita. 2011;47(3):278-83. PubMed | Google Scholar
- Woolf AD. Herbal remedies and children: do they work? Are they harmful? Pediatrics. 2003 Jul;112(1 Pt 2):240-6. PubMed | Google Scholar
- World Health Organisation. Updated guideline: paediatric emergency triage, assessment and treatment (ETAT). Accessed on May 26th, 2019.
- Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013 Apr;35(2):121-6. PubMed | Google Scholar
- Oyedeji GA. Socioeconomic and cultural background of hospitalized children in Ilesa. Niger J Paediatr. 1985;12:111-7. Google Scholar
- Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin. 2010 Nov;28(4):571-86. PubMed | Google Scholar
- Abiodun MT, Oluwafemi RO. Spectrum and outcome of neonatal emergencies seen in a free health-care program in South-Western Nigeria. Niger J Clin Pract. 2017 Mar;20(3):283-289. PubMed | Google Scholar
- Abdulraheem I, Parakoyi D. Factors affecting mothers' healthcare-seeking behavior for childhood illnesses in a rural Nigerian setting. Early Child Development and Care. 2009;179:671-683. Google Scholar
- Abdulkadir MB, Ibraheem RM, Johnson WB. Sociodemographic and clinical determinants of time to care-seeking among febrile children under-five in North-Central Nigeria. Oman Med J. 2015 Sep;30(5):331-5. PubMed | Google Scholar
- Isezuo KO, Onankpa BO, Adamu A, Jiya FB, Amodu-Sanni M. Socio-demographic factors associated with late presentation and outcome of febrile children admitted in a tertiary facility in North-Western Nigeria: a comparative study. Int J Pediatr Res. 2020; 6:063. Google Scholar
- Gregory CJ, Nasrollahzadeh F, Dharmar M, Parsapour K, Marcin JP. Comparison of critically ill and injured children transferred from referring hospitals versus in-house admissions. Pediatrics. 2008 Apr;121(4):e906-11. PubMed | Google Scholar
- Royal,C, McKerrow NH. A retrospective review of the transfer of critically ill children to tertiary care in KwaZulu-Natal Province, South Africa, S Afr.J Child Health.2015;9(4):112-118. Google Scholar
- D Gilpin, S Hancock. Referral and transfer of the critically ill child. BJA Education. 2016; 16(8):253-57. Google Scholar
- Adeboye MA, Adegboye OA, Abdulkarim AA, Eze EC, Saka MJ, Usman A et al. Amulets, bands and other traditional applications seen among Emergency and Neonatal Pediatric admissions in a tertiary centre, Nigeria. Oman Med J. 2011 Sep;26(5):337-41. PubMed | Google Scholar
- Kocaoglu C, Selma SE, Kilicarslan C, Arslan S. Fluid management in children with diarrhea-related hyponatremic-hypernatremic dehydration: a retrospective study of 83 children. Med Glas (Zenica). 2014 Feb;11(1):87-93. PubMed | Google Scholar











