Burden of non-communicable diseases in Tunisia, 1990-2017: results from the global burden of disease study
Houyem Khiari, Rym Mallekh, Ines Cherif, Mohamed Hsairi
Corresponding author: Houyem Khiari, Faculty of Medicine of Tunis, University of Tunis El Manar, Tunis, Tunisia 
Received: 29 Jul 2021 - Accepted: 04 Sep 2021 - Published: 28 Sep 2021
Domain: Non-Communicable diseases epidemiology
Keywords: Burden, non-communicable diseases, trend, Tunisia
©Houyem Khiari et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Houyem Khiari et al. Burden of non-communicable diseases in Tunisia, 1990-2017: results from the global burden of disease study. Pan African Medical Journal. 2021;40:62. [doi: 10.11604/pamj.2021.40.62.30980]
Available online at: https://www.panafrican-med-journal.com//content/article/40/62/full
Research 
Burden of non-communicable diseases in Tunisia, 1990-2017: results from the global burden of disease study
Burden of non-communicable diseases in Tunisia, 1990-2017: results from the global burden of disease study
Houyem Khiari1,&, ![]() Rym Mallekh1,
Rym Mallekh1, ![]() Ines Cherif1, Mohamed Hsairi1
Ines Cherif1, Mohamed Hsairi1
&Corresponding author
Introduction: non-communicable diseases (NCDs) are the leading cause of mortality and disability worldwide especially in developing countries such as Tunisia. We aimed to describe the national burden of non-communicable diseases in 2017 and to analyze disability-adjusted life year trends from 1990 to 2017 in Tunisia by cause and gender.
Methods: we used Joinpoint regression analysis to assess trends of the age standardized disability-adjusted life year rate from 1990 to 2017 and to determine average annual percentage change.
Results: non-communicable diseases accounted for 87.7% of total disability-adjusted life year in Tunisia in 2017. The five leading causes of this rate in Tunisia in 2017 were cardiovascular diseases, musculoskeletal disorders, neoplasms, mental disorders and neurological disorders. The trend of disability-adjusted life year rate of non-communicable diseases decreased significantly from 23403.2 per 100.000 (95% CI: 20830.2-26285.8) in 1990 to 18454.6 (95% CI: 15611.3-21555.4) in 2017, with a change of -0.9%; p=0.00. The decrease of the age standardized disability-adjusted life year rate concerned mainly cardiovascular diseases and neoplasms secondly. This decrease was more important in female (change=-1.1, p=0.00) in comparison to males (change=-0.7, p=0.00). On the other hand, the increase of the standardized disability-adjusted life year rate was related to musculoskeletal disorders, diabetes, kidney disorders and substance use disorders with a significant annual percentage change of 0.1%, 0.2% and 1.3% (p=0.00) respectively.
Conclusion: the implementation of the national strategy is the key solution to mitigate the impact of non-communicable diseases in Tunisia.
Non-communicable diseases (NCDs) are the leading cause of mortality and disability worldwide [1]. According to the World Health Organization (WHO), NCDs were responsible for 41 million deaths in the world, which is equal to 71% of all deaths in 2016, including 15 million people aged between 30 and 69 years [2-4]. The burden of NCDs is huge and is still rising worldwide [5,6]. However, the highest risks of dying from these diseases were observed in low and middle-income countries (LMIC) [7,8].
Disease burden of NCDs can be measured by different indicators such as the disability-adjusted life years (DALYs) which is the equivalent of losing one year in good health because of premature death or disease or disability [1]. In Tunisia, NCDs constitute also a major public health issue. According to the WHO, in 2016, NCDs were responsible for 86% of all causes of death (49% from cardiovascular diseases, 12% from cancer, 5% from chronic respiratory diseases and 5% from diabetes) and 16% of premature deaths between 30-70 years [9].
The global epidemic of NCDs was recognized by the United Nations (UN). Therefore, multisectoral national policies and plans were established, framed in the development of the Sustainable Development Goals (SDGs) for the prevention and control of NCDs to be achieved by 2030 [7]. Heads of state and government committed to develop national responses including to reduce by one third premature mortality from NCDs, to strengthen responses to reduce the harmful use of alcohol, to achieve universal health coverage (UHC), to strengthen the implementation of the WHO Framework Convention on Tobacco Control (FCTC), to support the research and development of vaccines and medicines for NCDs that primarily affect developing countries and to provide access to affordable essential medicines and vaccines for NCDs [10].
The WHO global NCDs action plan, implemented collectively between 2013 and 2020 in order to support national efforts by an international cooperation, follows on from commitments made by the United Nation (UN) political declaration on the prevention and control of NCDs. This action plan sets priorities, provides strategic guidance on how countries can apply the roadmap of commitments of the UN and contributes to progress on 9 global NCDs targets to be attained in 2025, including a 25% relative reduction in premature mortality from NCDs by 2025 [11]. In line with the WHO action plan, Tunisia carried out a national strategy for the prevention and control of NCDs for the 2018-2025 period [11]. Understanding global trends and changes in the leading causes of disease burden over time is crucial to assess the achievement of the national strategy targeted goals especially to reduce by 25% the premature mortality from NCDs by 2025 [12]. However, data on mortality are scant in Tunisia.
In this way, the present study aimed to describe the national burden of NCDs in 2017 and to analyze DALYs trends from 1990 to 2017, in Tunisia by cause and gender, using data from the global burden of disease study 2017 (GBD 2017) [13].
Study design and data sources: it was a descriptive study about DALYs trends by cause and gender from 1990 to 2017, in Tunisia. Due to the lack of exhaustive and recent data on death statistics in Tunisia, the source of data for this research was generated retrospectively from the global burden of diseases, injuries, and risk factors study (GBD) 2017 in accordance with the guidelines for accurate and transparent health estimates reporting [13].
To analyze DALYs trends, we extracted national estimates of numbers and age-standardized rate (ASR) of DALYs, years of life lost (YLLs) and years living with a disability (YLDs) with 95% uncertainty intervals (UIs), for every cause of death by NCDs, by sex and age group, from 1990 to 2017 in Tunisia using the GBD results tool [14,15].
The global burden of diseases data base: the GBD data base uses the disability-adjusted life-year (DALY) to measure the disease burden at the population level. DALYs are calculated by summing years of life lost (YLLs) due to premature mortality and years of life lived with disability (YLDs), thereby incorporating both fatal and non-fatal burden. YLLs were estimated using standard GBD methods whereby each death is multiplied by the normative standard life expectancy at each age. YLDs were estimated using sequelae prevalence and disability weights derived from population-based surveys [14,15]. All estimates generated in GBD were accompanied by 95% UIs, and age-specific death rate (ASDR) were estimated on the basis of the GBD world population age standard. According to the GBD data base, causes are classified into 4 levels. At level 1, there are three large cause groupings: communicable, maternal and neonatal conditions and nutritional deficiencies (CMNND); NCDs and injuries. At level 2 there are 21 disease and injury categories. The finest level of detail in causes is provided at levels 3 and 4. Causes reported within each level are mutually exclusive. Level 2 NCDs featured in GBD 2017 were: cardiovascular diseases (CVDs); neoplasms (cancers); chronic respiratory diseases; diabetes, urogenital, blood and endocrine disorders; neurological disorders; cirrhosis; digestive diseases; mental disorders; substance use disorders; musculoskeletal disorders; and other non-communicable diseases (including congenital anomalies, sense organ diseases, skin and subcutaneous diseases, and oral disorders) [13].
Statistical analysis: we used Joinpoint regression analysis to assess trends of the ASDR of NCDs from 1990 to 2017 and to determine average (mean) annual percentage change (APC) by a regressing log-linear function of the age-standardized DALYs per 100,000 population. APC was considered significant when it is different from zero at α=0.05. A constant trend was considered when the zero value was within both 95% UI limits for the APC, an increasing trend when both 95% UI limits were positive and a decreasing trend when both 95% UI limits were negative.
Ethical considerations: ethics approval was not required for this study.
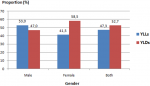
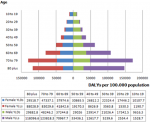
Burden of NCDs in Tunisia in 2017 by cause and gender: NCDs accounted for the highest proportion of disease burden in Tunisia in 2017 representing 87.7% of total DALYs; while, this proportion was of 8.6% and 5.1% for CMNND and injuries respectively. Among total of DALYS for NCDs, 52.7% were from YLDs. Females contributed to a larger proportion of YLDs than males; however, the reverse was observed for YLLs (Figure 1). For both genders, NCDs were responsible of 18454.6 DALYs per 100.000 (15611.3 - 21555.4) in 2017. The distribution of ASDR by gender was higher in males with 20167.2 DALYs per 100.000 versus 16818.3 in females. CVDs were the leading level 2 causes of NCDs burden contributing 5102.5 per 100.000 DALYs (4297.7 - 6008.8) which represented more than the quarter of toČtal ASDR (27.6%). CVDs were also the first leading cause groups of DALYs by gender, with 30.8% and 23.8% in males and females, respectively. The next most prominent causes were musculoskeletal disorders (MSD) (10.7%), neoplasms (10.0%), mental disorders (9.7%) and neurological disorders (8.7%) (Table 1). Comparison of genders, showed that the main difference of the most important level 2 cause groups of DALYs was for neoplasms; which were the second most common cause in males (11.1%) but the fifth ones in females (8.7%). A part from other NCDs, diabetes and kidney disorders and chronic respiratory diseases occupied the seventh and eighth place respectively (Table 1). According to the distribution analysis of DALYs by age groups, in both genders, the highest level of DALYs was observed in the 70-79 years age group, followed by 80 years and over, 60-69 years and 50-59 years age groups (Figure 2).
Trends of the ASDR of NCDs in Tunisia between 1990 and 2017: regarding the trend of the ASDR due to NCDs for all ages, it decreased significantly from 23403.2 per 100.000 (20830.2 - 26285.8) in 1990 to 18454.6 (15611.3 - 21555.4) in 2017, with an APC of -0.9%; p=0.00. This trend was mainly observed for CVDs (essentially ischemic heart disease and stroke) with a significant APC of -1.4% (-1.8%; -1.0%); p=0.00. This decrease was observed at a lesser degree for neoplasms; the ASDR decreased from 1937.7 (1821.4 - 2047.9) to 1842.5 (1518.1 - 2205.1) with a non-significant APC of -0.3%. Mental disorders, neurological disorders, chronic respiratory diseases and sense organ diseases showed also a significant declining trends of the ASDR with an APC respectively of -0.01%, -0.1%, -0.8% and -0.7%; p=0.00.
On the other hand, the increase of the ASDR was due to MSD, diabetes, kidney disorders and substance use disorders with a significant APC of 0.1%, 0.2% and 1.3% (p=0.00) respectively during the 1990-2017 period, and also for some cancers including the overall ASDR of NCDs decreased in both genders with an APC of -0.7% in males and -1.1% in females (p=0.00). The decrease for CVDs (APC of -1.1% in males vs -1.9% in females; p=0.00) and neoplasms (APC of -0.4% in females; p=0.00) was more important in female in comparison to males; in fact, the ASDR of hypertensive heart disease and some other CVDs (such as atrial fibrillation and flutter, endocarditis and peripheral artery disease), which dropped among females, significantly increased in males. The decrease of the ASDR of neoplasms was mainly in females with a significant APC of -0.4%; p=0.00. In females, cervical cancer showed a declining trend. However, breast cancer and tracheal, bronchus and lung cancer were on the rise. Concerning colorectal cancers, a non-significant ascending trend among both genders was observed (Table 2, Table 2 (suite), Table 2 (suite 1), Table 2 (suite 2), Table 2 (suite 3), Table 2 (suite 4)). MSD, the second most common cause of DALYs rate in 2017 (Table 1), showed an increasing ASDR with a significant APC of 0.1% in both genders. Thus, the ASDR of diabetes raised also significantly but essentially in males with an APC of 0.5%. Substance use disorders, concerned particularly drug use disorders with an APC of 1.7% and 1.0% in males and females respectively (Table 2, Table 2 (suite), Table 2 (suite 1), Table 2 (suite 2), Table 2 (suite 3), Table 2 (suite 4)).
The present study described the burden of NCDs in 2017 and analyzed DALYs trends by cause and gender in Tunisia during the 1990-2017 period, using data from the GBD [14]. According to this research, the burden of NCDs was very high; NCDs were responsible of 87.7% of the global ASDR; whereas only 8.6% were due to CMNND in 2017. The five leading level 2 causes of the ASDR of NCDs in Tunisia in 2017 were CVDs, MSD, neoplasms, mental and neurological disorders. Our findings have also shown that the trend of the ASDR of NCDs was significantly decreasing from 1990 to 2017, mainly for CVDs and at a lesser extent for neoplasms.
The declining trend of the burden of NCDs in Tunisia would be the result of treatment progress and a better management of patients, rather than the control of NCD´s risk factors. According to the WHO, more than 80% of NCDs can be prevented by eradicating the common risk factors, mainly tobacco use, unhealthy diets, physical inactivity and the harmful use of alcohol. Acting on modifiable causes of NCDs is the most cost-effective strategy to reduce the burden of NCDs and to improve longevity in the future [16]. In Tunisia, the prevalence of tobacco use remains high, despite the slightly decreasing trend during the period from 1990 (30%) to 2016 (25%) [17-19]; however, the prevalence of tobacco consumption was declining in almost all regions of the world [20]. Insufficient physical activity is one of the ten leading risk factors for global mortality due to NCDs. In Tunisia, more than the half (57.7%) of people aged over 15 years had insufficient physical activity [18]. The WHO mentioned that the East Mediterranean Region (EMR)(35%) had the highest prevalence of insufficient physical activity after the WHO region of America (39%) [21]. Food habits changes were the leading pattern of the life style shift, in line with the epidemiologic transition, WHO African and East Mediterranean Region (EMR) [22]. Principal dietary changes in Tunisia, between 1985 and 1995, were the reduction of the consumption of cereals, wheat, fish, fruits and vegetables against a rise intake of milk products, meat and fat [23]. In 2016, 80% of Tunisian aged over 15 years old did not consume enough fruits and vegetables per day [18]. Similar observations were described in the EMR, where dietary patterns consisted in low whole grains, low fruit, low vegetables and high sodium intake [24]. Obesity is also a real public health problem in Tunisia. In 2016, the average body mass index (BMI) in the population was of 26.9 ± 5.8 Kg/m2 which mean an overweight [18]. In addition, the trend of the prevalence of obesity in Tunisia had increased from 10.9% in 1998 to 26.9% in 2016 [25-27].
To fight against NCDs and their risk factors in Tunisia, many strategies and programs were set up such as the program for the control of diabetes and hypertension, the cancer plan, the national strategy against CVDs, the national program for tobacco control, the national strategy for the prevention and control of obesity 2013 - 2017 etc. but, these actions were sparse and lacked multi-sectoral coordination due to a deep problem of governance and leadership [28]. Thus, the national strategy for the control and prevention of NCDs (including CVDs, cancers, chronic respiratory disorders and diabetes), based on WHO NCDs control strategy aimed to control main risk factors of NCDs by the reduction of the harmful use of chronic alcohol consumption by at least 10%, the reduction by 10% of sedentarily, the reduction by 30% of tobacco and salt intake, the reduction by 30% of hypertension and the stabilization of the prevalence of diabetes and obesity [12]. However, due to lack of budget, this strategy has not yet been implemented. Currently in Tunisia as well as all other countries, health policy makers focused mainly on the control of COVID-19 pandemic, however, this should not lead to loosening of NCDs control strategy. The decreasing trend of the ASDR of NCDs stated by this study is consistent with previous studies in high-income and some middle-income countries [29]. Yet, it is important to mention that the decreasing trend of the ASDR of CVDs was not observed diabetes and hypertensive heart disease essentially among males.
Neoplasms showed also a global declining ASDR; nevertheless, there were some differences between genders; the decrease was observed only in females. Cervical cancer showed a declining trend; which could be the results of primary prevention and in a less degree of the screening program. However, the burden of breast cancer was on the rise. Concerning colorectal cancers, the ASDR in both genders was steady. In fact, according to the national cancer plan in Tunisia for the 2015-2019 period, cancer screening is opportunist with a low the coverage [30]. Given the rising trend of breast cancer and secondly colorectal cancers in Tunisia, screening strategies need to be strengthened and the existing pilot screening projects need to be provided with sufficient material and human resources. A better awareness of the population and health care providers is recommended.
On the other hand, a part of the increasing trend of NCDs burden was related to MSD which occupied the second rank broad cause groups of DALYs in females and the third one in males, in Tunisia in 2017. Population growth, aging and sedentary lifestyles, would have contributed to this trend [31]. It is important to mention that MSD share risk factors common to other NCDs, such as obesity, unhealthy diet and a sedentary lifestyle [32]. To our knowledge, this is the first study in Tunisia assessing the burden trend of NCDs for al causes and by gender which is very important to alert health policy makers for the urgent need for action to control NCDs burden in Tunisia. The main limitation of this study was related to the use of estimated data from the GBD rather than national data. However, national data of causes of death are not valid; on the other hand, the quality GBD data four countries is satisfactory.
Although the decreasing trend of NCDs burden in Tunisia from 1990 to 2017, mainly for CVD and neoplasms, this burden remains high. Reducing the levels of behavioral risk factors (tobacco use, physical inactivity, unhealthy diet) among Tunisian population are the key solutions to mitigate the impact of NCDs. A better governance for the implementation of the national strategy for the control and prevention of NCDs is urgently needed, underscoring the importance of leadership and the multisectoral coordination.
What is known about this topic
- Non-communicable diseases (NCDs) are the leading cause of mortality worldwide;
- The sustainable development goals include a target of a one-third reduction in premature mortality from NCDs by 2030 relative to 2015 levels;
- In line with the WHO action plan, Tunisia carried out a national strategy for the prevention and control of NCDs for the 2018-2025 period.
What this study adds
- This study describes and analyses global trends and changes of NCDs burden for al causes and by gender in Tunisia;
- This is very important to assess the achievement of the national strategy targeted goals and to alert health policy makers for the urgent need for action to control NCDs burden in Tunisia.
The authors declare no competing interests.
MH contributed to the conception and the study design; HK, RM and IC were involved in data extraction, analysis and interpretation; MH drafted and corrected the manuscript. All the authors have read and agreed to the final manuscript.
Table 1: ten leading broad cause groups of DALYs per 100.000 by gender, in Tunisia, 2017
Table 2: trends of age-standardized DALYs by gender: 1990 to 2017
Table 2 (suite): trends of age-standardized DALYs by gender: 1990 to 2017
Table 2 (suite 1): trends of age-standardized DALYs by gender: 1990 to 2017
Table 2 (suite 2): trends of age-standardized DALYs by gender: 1990 to 2017
Table 2 (suite 3): trends of age-standardized DALYs by gender: 1990 to 2017
Table 2 (suite 4): trends of age-standardized DALYs by gender: 1990 to 2017
Figure 1: YLLs and YLDs proportion by gender among NCDs in 2017 (YLLs: years of life lost due to premature mortality; YLDs: years lived with disability)
Figure 2: total disability-adjusted life years (DALYs) rates by gender and age group, Tunisia, 2017
- Richards NC, Gouda HN, Durham J, Rampatige R, Rodney A, Whittaker M. Disability, non-communicable disease and health information. Bull World Health Organ. 2016;94(3):230-232. PubMed | Google Scholar
- World Health Organization. Global health estimates 2016: deaths by cause, age, sex, by country and by region, 2000-2016. Geneva: WHO. 2018.
- Islam SM, Purnat TD, Phuong NT, Mwingira U, Schacht K, Fr÷schl G. Non-communicable diseases (NCDs) in developing countries: a symposium report. Globalization and Health. Global Health. 2014;10:81. PubMed | Google Scholar
- World Health Organization. Global action plan on physical activity 2018-2030: more active people for a healthier world. 2019. Google Scholar
- Boutayeb A. The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg. 2006;100(3):191-9. PubMed | Google Scholar
- Benziger CP, Roth GA, Moran AE. The global burden of disease atudy and the preventable burden of NCD. Glob Heart. 2016;11(4):393-7. PubMed | Google Scholar
- Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME et al. NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. The Lancet. 2018;392(10152):1072-88. PubMed | Google Scholar
- Vardell E. Global health observatory data repository. Med Ref Serv Q. 2020;39(1):67-74. PubMed | Google Scholar
- Andersen K, Gudnason V. Chronic non-communicable diseases: a global epidemic of the 21st century. Laeknabladid. 2012;98(11):591-595. PubMed | Google Scholar
- World Health Organization. WHO global coordination mechanism on the prevention and control of non-communicable deseases (GCM/NCD). 2017.
- World Health Organization. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. 2013. Google Scholar
- Abdelmajid BH, Dellagi RT, El Ati J, Hsairi M, Fakhfakh R, Gzara A et al. Stratégie nationale multisectorielle de prévention et contrôle des maladies non transmissibles (MNT) 2018-2025. Tunisia: WHO. 2018.
- Global Burden of Disease Collaborative Network. Global burden of disease study 2017 (GBD 2017) burden by risk 1990-2017. Seattle, United States: Institute for Health Metrics and Evaluation (IHME). 2018.
- Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray C. Measuring the global burden of disease and risk factors, 1990-2001. Global Burden of Disease and Risk Factors. 2006;1:1-14. PubMed | Google Scholar
- Murray CJ, Lopez AD. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. World Health Organization. 1996. Google Scholar
- World Health Organization. Global status report on non-communicable diseases 2014. 2014. Google Scholar
- Ben Romdhane H, Bougatef S, Skhiri H, Gharbi D, Kafsi MN, Belhani A et al. Le registre des maladies coronaires en Tunisie: organisation et premiers résultats: the first Tunisian cardiovascular diseases register: processes and results. Rev Epidemiol Sante Publique. 2004;52(6):558-64. PubMed | Google Scholar
- Saidi O, Zoghlami N, Skhiri H, Hsairi M, Skhiri A, Ben Mansour N et al. Tunisian health examination survey-2016. République Tunisienne: Ministère de la Santé, Institut National de la Santé. 2019.
- Fakhfakh R, Hsairi M, Maalej M, Achour N, Nacef T. Tabagisme en Tunisie: comportements et connaissances. Bull World Health Organ. 2002;80(5):350-356. PubMed | Google Scholar
- World Health Organization. WHO global report on trends in prevalence of tobacco smoking 2000-2025, second edition. Geneva: World Health Organization. 2018. Google Scholar
- Guthold R, Stevens GA, Riley LM, Bull FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 19 million participants. Lancet Glob Health. 2018;6(10):e1077-e1086. PubMed | Google Scholar
- Sibai AM, Nasreddine L, Mokdad AH, Adra N, Tabet M, Hwalla N. Nutrition transition and cardiovascular disease risk factors in Middle East and North Africa countries: reviewing the evidence. Ann Nutr Metab. 2010;57(3-4):193-203. PubMed | Google Scholar
- Ben Romdhane H, Khaldi R, Oueslati A, Skhiri H. Transition épidémiologique et transition alimentaire et nutritionnelle en Tunisie. Options Méditerranéennes. 2002;B41:7-27. Google Scholar
- Yu E, Malik VS, Hu FB. Cardiovascular disease prevention by diet modification: JACC health promotion series. J Am Coll Cardiol. 2018;72(8):914-926. PubMed | Google Scholar
- Elasmi M, Feki M, Sanhaji H, Jemaa R, Haj Taeib S, Omar S et al. Prévalence des facteurs de risque cardiovasculaires conventionnels dans la population du grand Tunis. Rev Epidemiol Sante Publique. 2009;57(2):87-92. PubMed | Google Scholar
- Ben Romdhane H, Ben Ali S, Skhiri H, Traissac P, Bougatef S, Maire B et al. Hypertension among Tunisian adults: results of the TAHINA project. Hypertens Res. 2012;35(3):341-7. PubMed | Google Scholar
- Traissac P, Beji C, Oueslati A, Gaigi S, Kolsteren, P, Delpeuch F et al. Overweight and obesity in Tunisia (Tahina project): trends over the last 25 years. Ann Nutr Metab. 2007;51(1). Google Scholar
- Ben Romdhane H, Tlili F, Skhiri A, Zaman S, Phillimore P. Health system challenges of NCDs in Tunisia. Int J Public Health. 2015;60 Suppl 1:S39-46. PubMed | Google Scholar
- Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J Am Coll Cardiol. 2017;70(1):1-25. PubMed | Google Scholar
- Hsairi M, Mehdi F, Bellaaj R, Kassis M. Health screening strategies in Maghreb countries: situation analysis and perspectives. Tunis Med. 2018;96(10-11):688-695. PubMed | Google Scholar
- Briggs AM, Cross MJ, Hoy DG, Sànchez-Riera L, Blyth FM, Woolf AD et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 World Health Organization world eeport on ageing and health. The Gerontologist. 2016;56 Suppl 2:S243-255. PubMed | Google Scholar
- Williams A, Kamper SJ, Wiggers JH, O'Brien KM, Lee H, Wolfenden L et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. PubMed | Google Scholar