Recurrent haemorrhagic ovarian cyst and anticoagulant therapy: a case report with review of treatment modalities
Kavitha Nagandla, Mohamed Faiz Bin Mohamed Jamli, Faridah Hanim, Joanne Lim Xu Mei, Siti Fathima Syazliana Din
Corresponding author: Kavitha Nagandla, Department of Obstetrics and Gynaecology, International Medical University, Clinical Campus, Jalan Rasah, 70300 Seremban, Negeri Sembilan, Malaysia 
Received: 28 Jul 2021 - Accepted: 03 Sep 2021 - Published: 21 Sep 2021
Domain: Gynecology
Keywords: Haemorrhagic, ovarian cyst, anticoagulants, management, surgery
©Kavitha Nagandla et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Kavitha Nagandla et al. Recurrent haemorrhagic ovarian cyst and anticoagulant therapy: a case report with review of treatment modalities. Pan African Medical Journal. 2021;40:52. [doi: 10.11604/pamj.2021.40.52.30961]
Available online at: https://www.panafrican-med-journal.com//content/article/40/52/full
Case report 
Recurrent haemorrhagic ovarian cyst and anticoagulant therapy: a case report with review of treatment modalities
Recurrent haemorrhagic ovarian cyst and anticoagulant therapy: a case report with review of treatment modalities
![]() Kavitha Nagandla1,&, Mohamed Faiz Bin Mohamed Jamli2, Faridah Hanim2, Joanne Lim Xu Mei2, Siti Fathima Syazliana Din2
Kavitha Nagandla1,&, Mohamed Faiz Bin Mohamed Jamli2, Faridah Hanim2, Joanne Lim Xu Mei2, Siti Fathima Syazliana Din2
&Corresponding author
The common gynaecological causes of acute pelvic pain include ruptured ectopic pregnancy, haemorrhagic corpus luteal cyst or torsion of an ovarian cyst. Ovarian vascular accidents are reported in women on oral anticoagulation presenting as an acute pelvic pain. Although such vascular accidents with anticoagulation therapy are an unusual entity, a meticulous history, clinical examination, and laboratory workup to confirm the diagnosis and timely intervention is needed to reduce attending morbidity and mortality. However, a standard algorithm for management is not described in the literature. We hereby report successful management of recurrent hemorrhagic ovarian cyst due to coagulopathy in a woman with mechanical heart valves with timely surgical intervention. This case report discusses operative versus non operative management approach and may provide value addition to readers encountering such cases in their clinical practice.
Women with mechanical prosthetic heart valves are considered high risk population with increased incidence of thromboembolic events [1]. Therapeutic anticoagulation as long-term measure is effective in preventing future thromboembolic episodes and their associated mortality [2]. Spontaneous bleeding is one of the most common adverse effects of warfarin, and factors such as old age, dose, duration of therapy, drug interaction and occult diseases further determine the risk of bleeding [3]. Strict monitoring of the coagulation profile is therefore paramount in patients taking long-term anticoagulation. Major gynecological bleeding complications from anticoagulation therapy although are rare, cases have been reported of hemorrhagic rupture of luteal cysts in premenopausal women in the absence of concurrent ovulation suppression [4]. The reported incidence of hemorrhagic ovarian cysts is 1% among women receiving anticoagulation medications and frequently a complication when International Normalized Ratio (INR) is more than 4 [5]. Life-threatening bleeding can occur with cystic hemorrhage from rupture, with an associated mortality rate from resultant hemoperitoneum of more than 11% [6]. Such patients present a challenge, as abrupt reversal of anticoagulation is required to control any ongoing hemorrhage and further surgical blood loss [7]. Currently, there are no clear recommendations regarding the modalities required to reverse anticoagulation for emergency surgery and the ideal time to restart anticoagulation therapy safely [7]. We describe a case of recurrent hemorrhagic ovarian cyst in premenopausal women with mechanical heart valves on anticoagulation therapy who presented in emergency with acute abdomen and was managed successfully with emergency exploratory laparotomy and adequate blood products.
Patient information: a 47-year-old nulliparous female presented to an emergency department with left lower abdominal pain for the last three days. She has an underlying history of chronic rheumatic heart disease and mitral valve replacement and is anticoagulant therapy with warfarin 2.5 mg once daily since 1994. She has underlying history of hypertension and diabetes mellitus which has been well controlled. She has a history of emergency laparotomy for haemorrhagic ovarian cyst in 2005 and cystectomy and bilateral tubal ligation performed as she was not keen for fertility in view of her underlying cardiac condition. Furthermore, she is diagnosed with bilateral endometrioma since 2018 and is on conservative management. Her last menstrual period was twenty days ago, with regular menstrual history and moderate flow.
Clinical findings: on examination, she was pale, and there is presence of diffuse tenderness on per abdominal examination. The cardiovascular examination revealed mechanical valve click, pulse rate of 108beats/minute blood pressure of 100/60 mm Hg. Per speculum revealed healthy cervix and on vaginal examination: uterus- normal-sized, anteverted, bilateral fornix-fullness present.
Diagnostic assessment: on initial laboratory work-up, she was noted to have a hemoglobin (Hb) of 10g/dL, hematocrit of 33.6%, and platelet count of 248, INR of 2.7 with normal prothrombin time and activated partial thromboplastin time. Urine pregnancy test was negative. An ultrasound scan of the pelvis revealed an adnexal lesion with mixed echogenic adnexal mass abutting the uterus. There is no free fluid seen. She developed a spike of fever on the second day of admission and septic workup was initiated. Her total white blood cells increased from 13.3 to 16.1cells/mm3.
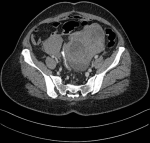
Diagnosis: a provisional diagnosis of infected endometrioma was made, and she was started on Intravenous cephalosporins. Her COVID polymerase chain reaction (PCR) was negative. An echocardiography showed normal functioning valves. She was afebrile 24 hours post antibiotic administration and a decision was made to manage her conservatively. On Day 4 of admission, her hemoglobin dropped to 6 g/dl. A computerized tomography of the pelvis revealed large bilateral adnexal masses with no active extravasation, indicating no active bleeding (Figure 1). However, INR was 6.6 and cardiology decision was to stop warfarin due to overanticoagulation related to concomitant drug interaction with cephalosporins and possible risk of ongoing hemorrhage.
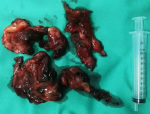
Therapeutic interventions: in view of acute anemia, she was planned for emergency laparotomy and total abdominal hysterectomy with bilateral salpingo-oophorectomy was proceeded as patient requested for a definitive management due to underlying cardiac condition. Preoperatively she was transfused with 2 units of whole blood and Intravenous vitamin K 2 mg for warfarin reversal. Intraoperative findings include bilateral adnexal masses, that ruptured on manipulation with 200-300cc clots from both the ovaries (Figure 2). During adhesiolysis of dense adhesions related to her previous surgery, there was an iatrogenic bladder and serosal tear of sigmoid colon and repair was performed respectively.
Follow-up and outcome of interventions: postoperatively, she was transfused with 2 units whole blood and monitored with daily INR. Her hemoglobin improved to 9 g/dl. In view of hematuria immediate postoperative period, and risk of bleeding, a decision was made to delay the initiation of anticoagulants. Her INR was 1.8-2.2 and she was started on subcutaneous low molecular weight heparin (LMWH) until 10th post-operative day and bridged with warfarin 2.5 mg following normalization of INR for at least 48 hours. She was discharged uneventfully on 14th post-operative day. Histopathology report was suggestive of haemorrhagic ovarian cyst.
Patient perspective: at 6 weeks follow-up in combined Gynaecology and Medical Clinic, she had normal bladder and bowel functions and had expressed satisfaction that a definitive treatment has been achieved. She had given the authors permission to publish this case report.
It is well known that patients with prosthetic heart valves require lifelong anticoagulation to prevent thromboembolic events [2]. However, prolonged anticoagulation presents with future complications such as significant bleeding diathesis that can be life-threatening requiring emergency interventions [3]. Bleeding conditions include gastrointestinal bleed, intracranial bleed, menorrhagia, and ovarian haemorrhage due to rupture of follicle or corpus luteum [2]. There are many published reports as case series of corpus luteal haemorrhage, however there are few reports addressing bleeding in women with mechanical heart valves [8-10]. Our case further adds to the literature. The overall estimated mortality in this group of patients has been reported as 3-11% and recurrence risk of 25-31% of cases [11]. It is paramount to have a close monitoring of coagulation profile in patients on long-term anticoagulants to prevent such complications.
Currently, there is no standard algorithm in the management of patients presenting with haemorrhagic ovarian cysts. Barel et al. reported abdominal pain as a prevalent and constant symptom in all patients; 10.7% also had fever, 13% had nausea and vomiting, and 4% showed urinary disorders [12]. It is worth mentioning that it is not always clinically possible to differentiate hemorrhagic cyst and ruptured hemorrhagic cyst. Although several previous studies have reported a rate of surgery for ruptured hemorrhagic cysts with hemoperitoneum as high as 80% [13]. Conservative management is usually performed with analgesia and close observation in actual clinical settings, which is supported by recent advances in imaging studies that allow an early and accurate diagnosis [14]. In a recent study, the role of pre-treatment computed tomography (CT) that can predict the necessity of surgical treatment based on image findings were reported. It is identified that presence of active bleeding and depth of hemoperitoneum on axial plane are potential risk factors for surgery in these patients [15].
The principles of treatment are aimed at controlling the bleeding and salvage the ovaries [14]. However, it is not always possible to adopt a conservative approach and surgical approach is restored in the event of hemodynamic instability or diagnostic dilemma similar to our case where the CT findings suggestive of adnexal cyst with no active bleeding [15]. A contrast-enhanced CT of the abdomen is recommended over ultrasound to initiate correct management in a timely fashion [15]. However, few observations in literature have challenged validity of surgical modality as first therapy. First, hemoperitoneum up to 1litre gets absorbed within a week and non-inflammatory ovarian bleeding is not associated with intra-abdominal adhesions [16].
If surgical modality is the option, there is ambiguity regarding the treatment to reverse anticoagulation for emergency surgery and the ideal time to restart anticoagulation therapy safely [7]. The possible options for reversal of anticoagulation include vitamin K, prothrombinase complex concentrate (PCC) and fresh frozen plasma (FFP) [3]. The most immediately available is FFP and vitamin K. It is identified that there is PCC-associated thrombotic risk because of high level of factor II in the PCC (relative to the other factors), which is known to increase thrombin generation especially in the situation of mechanical heart valves [3]. With regard to restarting anticoagulation in patients with warfarin-induced major bleeding and mechanical heart valves, the safe period varies from 7-14 d after the onset of bleeding [8]. As ovarian cyst hemorrhage may reoccur, ovulation suppression should be considered. There is a good evidence for prescribing depot medroxyprogesterone (DMPA) to suppress ovulation in anticoagulated patients with prosthetic heart valves [17]. However, in our case, there was no preceding formal recommendation of hormonal therapy for ovarian suppression.
Patients who are on oral anticoagulants have more chances of bleeding tendencies and higher risk of recurrences of haemorrhagic ovarian cyst. Massive hemoperitoneum resulting from an ovarian cyst rupture is rare, but potentially life-threatening if not diagnosed and treated emergently. Conservative management is an option in hemodynamically stable patients. However, a low threshold of surgical intervention must be the approach in the presence of diagnostic dilemma with emergency reversal of anticoagulation and restarting therapy postoperatively as guided by the potential risk of rebleeding. Although the risks of specific hormonal contraceptives in this patient population still warrant further investigation, hormonal contraception can be safe and efficacious therapy for ovulation suppression and prevention of future recurrences.
The authors declare no competing interests.
Conception and study design: KN and MFBMJ. Data collection: KN, JLXM and SFSD. Data analysis and interpretation: FH and KN. Manuscript drafting: KN and MFBMJ Manuscript revision: KN, MFBMJ and FH. Guarantor of the study: KN. All authors have read and agreed to the final manuscript.
Figure 1: computerized
tomography (CT) of pelvis showing bilateral enlarged irregular
heterogeneously enhancing masses; several cystic components seen
in the mass suggestive of
necrosis; no contrast extravasation suggestive of active bleeding
is seen
Figure 2: specimen of bilateral hemorrhagic ovarian cysts that ruptured that on intraoperative manipulation with 200-300cc clots
- Jensen AS, Idorn L, Nørager B, Vejlstrup N, Sondergaard L. Anticoagulation in adults with congenital heart disease: the who, the when and the how? Heart. 2015 Mar;101(6):424-9. PubMed | Google Scholar
- Khairy P, Fernandes SM, Mayer JE Jr, Triedman JK, Walsh EP, Lock JE et al. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation. 2008 Jan 1;117(1):85-92. PubMed | Google Scholar
- Yamakami LY, de Araujo DB, Silva CA, Baracat EC, de Carvalho JF. Severe hemorrhagic corpus luteum complicating anticoagulation in antiphospholipid syndrome. Lupus. 2011 Apr;20(5):523-6. PubMed | Google Scholar
- Trenor CC 3rd, Chung RJ, Michelson AD, Neufeld EJ, Gordon CM, Laufer MR et al. Hormonal contraception and thrombotic risk: a multidisciplinary approach. Pediatrics. 2011 Feb;127(2):347-57. PubMed | Google Scholar
- Gupta A, Gupta S, Manaktala U, Gupta MM, Solanki V. Conservative management of corpus luteum haemorrhage in patients on anticoagulation: a report of three cases and review of literature. Arch Gynecol Obstet. 2015 Feb;291(2):427-31. PubMed | Google Scholar
- Curtis R, Schweitzer A, van Vlymen J. Reversal of warfarin anticoagulation for urgent surgical procedures. Can J Anaesth. 2015 Jun; 62(6):634-49. PubMed | Google Scholar
- Panduranga P, Al-Mukhaini M, Al-Muslahi M, Haque MA, Shehab A. Management dilemmas in patients with mechanical heart valves and warfarin-induced major bleeding. World J Cardiol. 2012 Mar 26;4(3):54-9. PubMed | Google Scholar
- Jamal A, Mesdaghinia S. Ruptured corpus luteum cysts and anticoagulant therapy.Int J Gynecol Obstet. 2002 Mar;76(3):319-20. PubMed | Google Scholar
- Payne JH, Maclean RM, Hampton KK, Baxter AJ, Makris M. Hemoperitoneum associated with ovulation in women with bleeding disorders: the case for conservative management and the role of the contraceptive pill. Hemophilia. 2007 Jan;13(1):93-7. PubMed | Google Scholar
- Ho WK, Wang YF, Wu HH, Tsai HD, Chen TH, Chen M. Ruptured corpus luteum with hemoperitoneum: case characteristics and demographic changes over time. Taiwan J Obstet Gynecol. 2009 Jun;48(2):108-12. PubMed
- Barel O, Smorgick N, Pansky M, Schneider D, Halperin R. Clinical and laboratory presentation of hemorrhagic corpus luteum. J Gynecol Surg. 2008;24:1. Google Scholar
- Gupta N, Dadhwal V, Deka D, Jain SK, Mittal S. Corpus luteum hemorrhage: rare complication of congenital and acquired coagulation abnormalities. The Journal of Obstetrics and Gynaecology Research. 2007 Jun;33(3):376-380. PubMed | Google Scholar
- Kim JH, Lee SM, Lee JH, Jo YR, Moon MH, Shin J et al. Successful conservative management of ruptured ovarian cysts with hemoperitoneum in healthy women. PLoS One. 2014 Mar 7;9(3):e91171. PubMed | Google Scholar
- Lee MS, Moon MH, Woo H, Sung CK, Jeon HW, Lee TS. Ruptured corpus luteal cyst: prediction of clinical outcomes with CT. Korean J Radiol. 2017 Jul-Aug;18(4):607-6. PubMed | Google Scholar
- Murao, H. Kinjyo, K. DemuraT. Conservative therapy for corpus luteum hemorrhage, a review of 116 cases. Clin Gynecol Obstet.1994;48:568-572. PubMed | Google Scholar
- Sonmezer M, Atabekoglu C, Cengiz B, Dokmeci F, Cengiz SD. Depot-medroxyprogesterone acetate in anticoagulated patients with previous hemorrhagic corpus luteum. Eur J Contracept Reprod Health Care. 2005 Mar;10(1):9-14. PubMed | Google Scholar
- Yoke Fai Fong, Hui Wen Chua, Chanchal Singh, Shi Hui Tan. Diagnostic dilemma: acute abdomen from ruptured corpus luteum requiring surgical intervention in young women Thai Journal of Obstetrics and Gynaecology. June 2013;21:2. Google Scholar