An outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria: a quasi-experimental study
Catherine Olukemi Agbede, Ugochinyere Chinasa Ekeanyanwu
Corresponding author: Ugochinyere Chinasa Ekeanyanwu, Department of Public Health, Babcock Unversity, Ilishan Remo, Ogun State, Nigeria 
Received: 30 Jun 2021 - Accepted: 01 Sep 2021 - Published: 08 Dec 2021
Domain: Health education,Health promotion,Public health
Keywords: Adolescent girls, menstrual hygiene, practices, peer-led, parent-led, health belief model
©Catherine Olukemi Agbede et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Catherine Olukemi Agbede et al. An outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria: a quasi-experimental study. Pan African Medical Journal. 2021;40:214. [doi: 10.11604/pamj.2021.40.214.30601]
Available online at: https://www.panafrican-med-journal.com//content/article/40/214/full
Research 
An outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria: a quasi-experimental study
An outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria: a quasi-experimental study
Catherine Olukemi Agbede1, Ugochinyere Chinasa Ekeanyanwu1,&
&Corresponding author
Introduction: adolescence is a special period of physical and psychological preparation for safe motherhood that requires specific attention as it marks the onset of menarche. Hygiene-related practices are significant during menstruation to prevent being predisposed to reproductive tract infections and other complications. The main objective of the study was to determine the outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria using the health belief model. One hypothesis guided the study.
Methods: the study utilized a quasi-experimental design comprising of three experimental groups and one control group. The population of the study was one hundred and twenty (120) in-school adolescent girls. The multistage sampling technique was used in selecting participants from four secondary schools within Ogun State. A validated semi-structured questionnaire was used for data collection with a Cronbach alpha with a score of 0.87. Data collected were analysed using Statistical Package for Social Sciences (SPSS) version 23.
Results: a paired T-test analysis was conducted in determining the results. The observed difference in the mean in the parent-led (Δ = 3.80; t = 20.886; p=0.000), peer-led group (∆ = 4.23; t = 19.901; p=0.000), and combination of parent and peer-led group intervention group (Δ = 3.53; t = 18.015; p=0.000) were statistically significant.
Conclusion: peer-led experimental group had the greatest effective change in the level of adolescent girls´ menstrual hygiene practices. Peer educators could be recruited for future interventions and scaled up in other aspects of young girls´ reproductive health and well-being.
Adolescence is a special period of physical and psychological preparation for safe motherhood that requires specific attention as it marks the onset of menarche [1]. According to the United Nations Children Fund (UNICEF), an adolescent is defined as any person between the ages of 10-19 years [2]. Globally, about 1.2 billion adolescents are of this age and 85% live in developing nations [2,3]. During menstruation, hygiene-related practices are fundamental particularly at the onset [4]. Good hygienic practices require the use of sanitary pads, washing of the body and genital areas, frequently changing of menstrual absorbents as well as proper disposal of used menstrual absorbents [5]. This will enhance the confidence of females in various aspects [6]. On the other hand, if proper hygiene is not practiced during a menstrual period, it could lead to poor academic performance, school dropout, and predispose one to reproductive tract infections (RTIs), pelvic inflammatory diseases, and other complications like carcinoma of the cervix and infertility problems [5,6]. Currently, the global prevalence of RTIs and their complications is unacceptably high between 15-80% in most impoverished communities [7]. Research has shown that women and adolescents girls with poor menstrual hygiene are three times more likely to have RTI than those with proper and adequate menstrual hygiene [8]. The World Health Organisation (WHO) acknowledges that about 80% of the global burden lies in low- and middle-income countries especially in the rural settlements as a result of ignorance and inadequate support for managing menstruation [9,10].
In Nigeria, over 10 million children mostly adolescent girls are already out of school due to access to adequate safe menstrual hygienic products and approximately 25 percent lack adequate privacy for defecation and menstrual hygiene management [11,12]. Researchers have discovered between 31 and 56% of schoolgirls in Nigeria using toilet tissue, cotton wool, or cloth to absorb menstrual blood as opposed to sanitary pads [13]. Learning about menstrual hygiene-related practices is a significant part of health education for adolescent girls [14]. This could enable them to continue to work and keep up with hygienic habits during their adult life. It will also help to improve maternal health; which can have an impact on the sustainable development goals (SDGs) for example SDG 3 [14]. The Health belief model (HBM) was espoused for this study. This model states that a stimulus or cue to action must be present to trigger the health-promoting behaviour [15]. However, this has been used in assessing underlying menstrual hygiene-related practices of adolescent girls and also has been used to inform the development of interventions to improve health behaviours [16,17]. Hence, this study needed to be conducted to determine the outcome of educational intervention on the menstrual hygiene practices among school girls in Ogun State, Nigeria. The study postulated that there will be no significant difference in the level of menstrual hygiene practices among in-school female adolescents between the baseline and 6-weeks follow-up.
Study design: the study was a school-based, quasi-experimental study comprising of three experimental groups and a control group using a quantitative approach. The three experimental groups were peer-led, parent-led, and a combination of both. The study encompassed a health education programme that was based on menstrual hygiene-related practices. The health education programme was delivered to the experimental groups and a placebo on COVID-19 prevention was delivered to the control group. Data were collected across the four groups before the program and at 4 weeks´ immediate post-intervention as well as at 6-weeks follow-up.
Study area and population: the present research was conducted in a rural area of Ogun State. Ogun State is located in the South-West and is situated between latitude 6.2°N and 7.8°N, and longitude 3.0°E and 5.0°E. It has an estimated 2016 population of 7.2 million and is predominantly covered by tropical rainforest and has a wooded savannah in the Northwest. There are about two hundred and ninety-one (291) public secondary schools and one hundred and eleven owned private secondary schools. The tertiary institutions both public and private are about twenty-one (21) making it the highest in the country. There are also twenty local government areas in Ogun State consisting of cities, towns, and villages. The study population comprised of in-school adolescent girls aged 10-19.
Inclusion and exclusion criteria: in-school adolescent girls in a rural area who attained menarche and were between the ages of 10-19; who were present on the day of the study and whose parents gave consent and were willing to take part in the study. In-school adolescent girls who are not in a rural area who did not attain menarche; who were below and above 10-19 years of age and whose parents did not give consent and were not willing to take part in the study.
Sampling technique: the multistage sampling technique was used in selecting the participants. A senatorial district in Ogun State was purposively selected; from the senatorial district, four local government areas were randomly selected after which a public secondary each was randomly chosen through balloting from the selected local government areas.
Sample size: a total of one hundred and twenty adolescent girls were selected for the study. The sample size was derived from the computation using a level of significance of 95% and 80% power. There was no given estimate of the prevalence of poor menstrual hygiene in secondary school female adolescents in Ogun State. Thus, the sample size was determined using the prevalence at 50%. The sample size was derived from the computation using a level of significance of 95% and 80% power. There was no given estimate of the prevalence of poor menstrual hygiene in secondary school adolescent girls´ in Ogun State.
Thus, the sample size was determined using the prevalence at 50%.
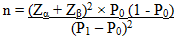
Where n is the minimum sample size per group Zα = 95% confidence interval i.e. 1.96; Zβ = 80% i.e. 0.84 (power to detect changes in the outcome variable and avoid type II error) P0 = prevalence (at 50%); P1 = 80% (desired level of outcome variable);
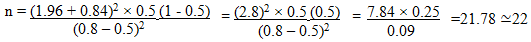
The minimum sample size was 22. Ten percent was added to the minimum sample size to take care of attrition. The total number of participants after adding 10% of 22 was 22 + 2.2 = 24 ≃30. Based on the computation a total number of 120 participants (30 per group x 4) was considered for the study (representing 30 people per group). Instrument for data collection. A semi-structured questionnaire made up of multiple-choice questions that sought information regarding socio-demographic characteristics and menstrual hygiene practices of participants was utilized for the study. The semi-structured questionnaire was designed after a review of the literature [18-21].
Validity and reliability: face validity of the instrument was adopted, and this was checked by faculty members. Content validity was also adopted by incorporating items identified in the literature review. To ascertain the reliability of the instrument, a pilot test was conducted for internal consistency of the instrument using 10% of the anticipated sample size using adolescent girls with the same characteristics. The data were statistically analyzed using the Cronbach alpha standard score to test its reliability. The reliability score generated was 0.87.
Data analysis: the data from the study were collated, entered, and coded using. Statistical Package for Social Sciences (SPSS) version 23. Data were presented using descriptive and inferential statistics and a statistical level of significance was set at p<0.05
Ethical approval and informed consent: ethical approval was obtained from Babcock University Health Research and Ethics Committee; the Ministry of Education Planning Research and Statistics, and the Ministry of Health Research Ethics, Ogun State. Written informed consent was obtained from the participants and their parents (mothers) explaining the aim of the research.
One hundred and twenty in-school adolescent girls were recruited from four junior and senior secondary schools in four local government areas in Ogun State, Nigeria. At baseline, the experimental groups and the control group each had an equal amount of 30 participants. The response rate across the four groups was 100% after the health education intervention was administered. There were more in-school adolescent girls in the middle adolescence (14-16 years) age bracket across the three experimental groups. The overall mean ± SD age of the adolescent girls recruited into this study was 14.92 ± 1.82 years and the mean ± SD age at menarche in this study was 12.73 ± 1.38 years. The adolescent girls were recruited from all secondary classes except SS3. The majority were Christians and only a few were reported to be a traditionalist. The ethnic distribution showed that the majority of the adolescent girls were from the Yoruba ethnic group and a few from the Igbo, Hausa, and other ethnic groups. The findings also disclosed that the majority of adolescent girls´ mothers had at least secondary or tertiary education and were businesswomen or traders (Table 1). The majority of participants across the three experimental groups and the control group reported to have been aware of menstrual hygiene and the information was sourced from mothers, teachers, sisters, and relatives (Table 2).
Baseline distribution of adolescents girls´ menstrual hygiene practices: the menstrual hygiene practices of adolescent girls were measured on a 7-point rating scale. The responses were grouped and the results showed that across the four groups, the majority of the adolescent girls in the parent-led group, peer-led group, parent and peer-led group, and control group had a low level of practice of menstrual hygiene behaviors. The mean ± SD scores for each group at baseline were 2.10 ± 0.995, 1.70 ± 1.12, 2.47 ± 0.94, and 2.10 ± 1.30 (Table 3).
The outcome of educational intervention of adolescent girls practice of menstrual hygiene: the outcome of the intervention of in-school adolescent girls practice of menstrual hygiene was assessed at immediate post-intervention and the results showed changes in the mean scores across the four groups parent-led, peer-led, parent and peer-led intervention, and control groups were statistically significant at p= 0.000. The outcome was also assessed at 6th-week follow-up and the results showed that there were changes in the mean score across the four groups. The evaluation indicated that the adolescent girls in the three experimental groups scored between 3.51- and 7-points and the combination of parent and peer-led intervention groups recorded the highest mean score (Table 3).
Change in the level of menstrual hygiene practices at baseline to 6-weeks follow-up: at the end of the intervention, the peer-led group had a statistically significant change in the mean of the adolescent girls' level of menstrual hygiene practices. The observed mean difference was 4.23 (p = 0.000). In the parent-led group, the mean difference was 3.80 (p= 0.000); while the combination of both was 3.53 (p= 0.000). There was a decrease of 0.20 in the control group which was also statistically significant (Table 4).
Research hypothesis: there will be no significant difference in the level of menstrual hygiene practices among in-school adolescent girls between the baseline and 6-weeks follow-up. To determine the results, a paired T-test analysis was conducted. The results showed that the observed difference in the mean in the parent-led (Δ= 3.80; t = 20.886; p= 0.000), peer-led group (Δ = 4.23; t = 19.901; p = 0.000), and combination of parent and peer-led group intervention group (Δ = 3.53; t = 18.015; p= 0.000) were statistically significant (Table 4). The results reveal that the educational interventions had an impact on the menstrual hygiene practices of the in-school adolescent girls in the three experimental groups, hence, the null hypothesis is rejected in favour of the alternative hypothesis (Table 4).
The present study shows that the age of participants across the four groups ranges from 10-19 years with the mean of 14.92 ± 1.82 years and majority of the girls being 14-16 which is comparable and similar to the age of high school adolescent girls reported in Saifai, Etawah, India [22], Saoner, Nagpur District, India [23] and Cross River State, Nigeria [24]. The mean age of menarche in the present study was 12.73 ± 1.38 years which is similar to the mean age reported among girls in Southwest Nigeria [25] but lower compared to findings conducted in District Sambhal, India [26]. The disparity in the mean age at menarche could be attributed to genetic, nutritional, and socioeconomic factors and general health; malnutrition, high level of physical activity, and chronic disease can as well delay menarche [22]. Hygienic-related practices are fundamental during menstruation as poor hygiene affects health by increasing vulnerability to infections of the reproductive and urinary tract [4-6]. The present study demonstrates that the level of menstrual hygiene practices of adolescent girls in the parent-led, peer-led, combination of parent and peer-led group, and the control group had a low level of practice of menstrual hygiene behaviors before the intervention. In the post-intervention, there was a significant improvement in the level of menstrual hygiene behaviours among the adolescent girls across the experimental groups compared to the control group. This finding agrees with the results of other studies in Bangladesh, Uyo, and Illorin, Nigeria [14,27,28]. There was also an increase in the mean scores of the adolescent girls´ menstrual hygiene practices at the 6th-week follow-up. This implies that students who underwent the educational intervention program had increased menstrual hygiene practices at the follow-up evaluation period. Therefore, it is appropriate to conclude that the educational intervention was effective in enhancing participants´ menstrual hygiene practices. Other researchers may develop interventions for out-of-school adolescents girls on menstrual hygiene practices and prevention of reproductive health infections.
Limitations: the findings of this study may be based on traditional, socio-economic, and cultural factors which influence the adoption of healthy behaviors in communities. The use of the findings of this study as a representation of adolescent girls in Nigeria may be limited due to the factors mentioned above.
The study revealed significant differences in the level of adolescent girls´ menstrual hygiene practices between baseline and follow-up periods. The peer-led experimental group had the greatest change. This implies that the use of peers in the school setting was effective in impacting better practices of menstrual hygiene and this could be recruited for future intervention and be scaled up in other aspects of young girls´ reproductive health and well-being.
What is known about this topic
- Hygiene-related practices are significant during menstruation to prevent being predisposed to reproductive tract infections and other complications;
- Majority of the global burden of reproductive tract infections lies in low- and middle-income countries especially in the rural settlements;
- Researchers have discovered between 31 and 56% of school girls in Nigeria using toilet tissue, cotton wool, or cloth to absorb menstrual blood as opposed to sanitary pads.
What this study adds
- The study added that the level of practice of menstrual hygiene behaviors was lower at a baseline level of assessment and the post-intervention, had a significant improvement in the level of menstrual behaviours which at the follow-up, there were also significant changes;
- Having a theory-based and a combination of interventions is effective in influencing a change in behaviors as revealed by the findings of this study.
The authors declare no competing interests.
Catherine Olukemi Agbede and Ugochinyere Chinasa Ekeanyanwu: conceptualized the study and were involved in the data collection process. All authors were involved in the data analysis and interpretation as well as the draft and final approval of the manuscript. All the authors have read and agreed to the final manuscript.
The authors are grateful to God Almighty for the enablement to complete this research work successfully. They are also grateful to the study participants from Ogun State, Nigeria for their support and cooperation.
Table 1: baseline distribution of socio-demographic characteristics of adolescents in control and intervention groups: age, age at menarche, class, religion, ethnic group, mother's level of education and mother' occupation
Table 2: baseline distribution of female adolescents´ menstrual hygiene awareness in experimental and control groups
Table 3: comparison of adolescent girls practice of menstrual hygiene at baseline, post-intervention and 6th- week follow-up for experimental and control groups
Table 4: change in the level of menstrual hygiene practices at baseline to 6-weeks follow up
- Kapoor G, Kumar D. Menstrual hygiene: knowledge and practice among adolescent school girls in rural settings. Int J Reprod Contracept Obstet Gynecol. 2017 Mar 1;6(3):959-63. Google Scholar
- United Nations Children Fund. UNICEF programme guidance for the second decade: programming with and for adolescents. 2018.
- Ilo CI, Nwimo IO, Onwunaka C. Menstrual hygiene practices and sources of menstrual hygiene information among adolescent secondary school girls in Abakaliki education zone of Ebonyi State. Journal of Education and Practice. 2016;7(31):88-95. Google Scholar
- Berhe H, Bayray A, Ukbayohannes R, Getachew G. Menstrual hygiene practice and associated factors among adolescent high school girls. Journal of Bio-Innovation. 2016;5(1):1-5.
- Bhusal CK. Practice of menstrual hygiene and associated factors among adolescent school girls in Dang district, Nepal. Adv Prev Med. 2020 Jul 24;2020:1292070. PubMed | Google Scholar
- Mohammed S, Larsen-Reindorf RE, Awal I. Menstrual hygiene management and school absenteeism among adolescents in Ghana: results from a school-based cross- study in a rural community. Int J Reprod Med. 2020 Apr 27;2020:6872491. PubMed | Google Scholar
- Kafle P, Bhattarai S. Prevalence and factors associated with reproductive tract infections in Gongolia village, Rupandehi District, Nepal. Advances in Public Health. 2016 Jan 1;2016. Google Scholar
- Almeida-Velasco A, Sivakami M. Menstrual hygiene management and reproductive tract infections: a comparison between rural and urban India. Waterlines. 2019 Apr 1;38(2):94-112. Google Scholar
- Kerubo E, Laserson KF, Otecko N, Odhiambo C, Mason L, Nyothach E et al. Prevalence of reproductive tract infections and the predictive value of girls´ symptom-based reporting: findings from a cross-sectional survey in rural western Kenya. Sex Transm Infect. 2016 Jun;92(4):251-6. PubMed | Google Scholar
- MacRae ER, Clasen T, Dasmohapatra M, Caruso BA. 'It´s like a burden on the head': redefining adequate menstrual hygiene management throughout women´s varied life stages in Odisha, India. PLoS One. 2019 Aug 1;14(8):e0220114. PubMed | Google Scholar
- Ball E. The urgent need to break Nigeria´s menstruation taboo. Humanitarian Aid Relief Trust. 2017.
- World Bank. Menstrual hygiene management enables women and girls to reach their full potential. 2018.
- Upashe SP, Tekelab T, Mekonnen J. Assessment of knowledge and practice of menstrual hygiene among high school girls in Western Ethiopia. BMC Womens Health. 2015 Oct 14;15:84 PubMed | Google Scholar
- Haque SE, Rahman M, Itsuko K, Mutahara M, Sakisaka K. The effect of a school-based educational intervention on menstrual health: an intervention study among adolescent girls in Bangladesh. BMJ Open. 2014 Jul 3;4(7):e004607. PubMed | Google Scholar
- Urich A. The health belief model. Accessed June 23, 2021.
- Kamal M, El-Borgy M, Wahba M. Application of health belief model for hygienic behavior of mothers of hospitalized children in Alexandria. Journal of High Institute of Public Health. 2017 Apr 1;47(1):13-21. Google Scholar
- Jones CJ, Smith H, Llewellyn C. Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review. Health Psychol Rev. 2014;8(3):253-69. PubMed | Google Scholar
- Ehianu A. Knowledge, perception and practices relating to menstruation among adolescents in public secondary schools in Ibadan North local government Area, Nigeria. 2017. Google Scholar
- Esther AU. Knowledge and management of menstruation and menstrual problems among urban and rural secondary school girls in Enugu East local government. 2016. Google Scholar
- Wanjiku D. Knowledge attitude and practices of menstrual hygiene among adolescent girls between S1-S4 St. Aloysius Bwanda Secondary School Kalungu. Doctoral dissertation, International Health Sciences University. 2016. Google Scholar
- Yadav RN, Joshi S, Poudel R, Pandeya P. Knowledge, attitude, and practice on menstrual hygiene management among school adolescents. J Nepal Health Res Counc. 2018 Jan 1;15(3):212-216. PubMed | Google Scholar
- Dixit AM. A cross-sectional study on menstrual hygiene practices among school going adolescent girls (10-19 years) of government girls inter college, Saifai, Etawah. International Journal Of Community Medicine And Public Health. 2018 Oct;5(10):4560. Google Scholar
- Thakre SB, Thakre SS, Reddy M, Rathi N, Pathak K, Ughade S. Menstrual hygiene: knowledge and practice among adolescent school girls of Saoner, Nagpur district. J Clin Diagn Res. 2011 Oct 1;5(5):1027-33. Google Scholar
- Edet OB, Bassey PE, Esienumoh EE, Ndep AO. An exploratory study of menstruation and menstrual hygiene knowledge among adolescents in urban and rural secondary schools in cross river State, Nigeria. African Journal of Biomedical Research. 2020 Sep 30;23(3):321-6. Google Scholar
- Fehintola FO, Fehintola AO, Aremu AO, Idowu A, Ogunlaja OA, Ogunlaja IP. Assessment of knowledge, attitude and practice about menstruation and menstrual hygiene among secondary high school girls in Ogbomoso, Oyo state, Nigeria. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2017 May;6(5):1726-32. Google Scholar
- Gupta S. An empirical study of managing menstrual hygiene in schools (a special reference to government upper primary schools in District Sambhal (Uttar Pradesh). Integrated Journal of Social Sciences. 2019 Jun 6;6(2):39-43. Google Scholar
- Ekong I. Effect of health education on menstrual hygiene and healthseeking behaviour among rural and urban adolescents. International Journal of Current Research and Review. 2015 Jul 15;7(14):27. Google Scholar
- Osinubi MO. Effect of peer education on menstrual hygiene knowledge and practices among adolescent girls in secondary schools in Ilorin, Kwara State. Public health. 2015. Google Scholar











