Hypercholesterolemia and related risk factors in a cohort of patients with diabetes and hypertension in Maputo, Mozambique
Fausto Ciccacci, Noorjehan Majid, Sandro Petrolati, Mustafa Agy, Cacilda Massango, Stefano Orlando, Giovanni Guidotti, Paola Scarcella, Maria Cristina Marazzi
Corresponding author: Fausto Ciccacci, UniCamillus, Saint Camillus International University of Health Sciences, Rome, Italy 
Received: 03 Dec 2020 - Accepted: 05 Dec 2020 - Published: 29 Jan 2021
Domain: Non-Communicable diseases epidemiology,Cardiology,Chronic disease prevention
Keywords: Hypercholesterolemia, non-communicable diseases, cardiovascular risk factor
©Fausto Ciccacci et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Fausto Ciccacci et al. Hypercholesterolemia and related risk factors in a cohort of patients with diabetes and hypertension in Maputo, Mozambique. Pan African Medical Journal. 2021;38:102. [doi: 10.11604/pamj.2021.38.102.27284]
Available online at: https://www.panafrican-med-journal.com//content/article/38/102/full
Research 
Hypercholesterolemia and related risk factors in a cohort of patients with diabetes and hypertension in Maputo, Mozambique
Hypercholesterolemia and related risk factors in a cohort of patients with diabetes and hypertension in Maputo, Mozambique
![]() Fausto Ciccacci1,&, Noorjehan Majid2,
Fausto Ciccacci1,&, Noorjehan Majid2, ![]() Sandro Petrolati3,
Sandro Petrolati3, ![]() Mustafa Agy2, Cacilda Massango2,
Mustafa Agy2, Cacilda Massango2, ![]() Stefano Orlando4,
Stefano Orlando4, ![]() Giovanni Guidotti5,
Giovanni Guidotti5, ![]() Paola Scarcella4,
Paola Scarcella4, ![]() Maria Cristina Marazzi6
Maria Cristina Marazzi6
&Corresponding author
Introduction: some studies reported that 25.5% of African population presents hypercholesterolemia; however, epidemiology of hypercholesterolemia in Africa is poorly described. Mozambique is experiencing a constant growth of non-communicable diseases, but scarce data are available about hypercholesterolemia. Our study aims at describing the prevalence of hypercholesterolemia in patients with diabetes and hypertension in Mozambique and investigate possible risk factors.
Methods: we conducted a cross-sectional study involving all the patients diagnosed with hypertension and/or diabetes from June 2018 to November 2020 in the Zimpeto DREAM Centre (Maputo, Mozambique). For each patient, anthropometric, clinical and laboratory data were collected. Hypercholesterolemia was defined as total blood cholesterol >200 mg/dL. Univariable and multivariable analysis were perfumed.
Results: a total of 885 patients were included, 76.2% (n=674) female. Hypertension alone was diagnosed in 670 (75.7%) patients, diabetes in 109 (12.3%) patients and 106 (11.9%) both diseases. Hypercholesterolemia was present in 410 (46.3%) patients and it was more prevalent in patients diagnosed with both diabetes and hypertension (52.8%), as compared to the patients diagnosed with hypertension (46.9%) or diabetes alone (36.7%). In the multivariable analysis, the only factors independently associated with hypercholesterolemia were female sex (aOR 1.77, 95% CI 1.26-2.48, p=0.001) and a body mass index >25kg/m2 (aOR 1.50, 95% CI 1.11-2.04, p=0.008).
Conclusion: our results highlight the need for a specific focus on female and obese/overweight patients, especially if diagnosed with both hypertension and diabetes, to promptly detect metabolic disorders and establish temporary preventive measures for cardiovascular events.
According to the World Health Organization (WHO), a third of the global burden of ischemic heart disease is attributable to hypercholesterolemia, that represents a fundamental challenge for global health [1]. Prevalence of hypercholesterolemiain African countries is poorly described. According to some authors, the general prevalence in Africa is 25.5% [2]. In many low- and middle-income countries, surveillance and research on non-communicable diseases are still lacking [3,4]. However, the number of NCDs-related deaths is dramatically rising in the last decades [5,6]. Many observers claimed for action to control non-communicable diseases (NCDs) in Africa [7,8].
Mozambique is experiencing a constant growth of NCDs incidence and mortality in recent years, although infectious diseases are still burdening the country [9]. The prevalence of hypercholesterolemia is in line with that of the continent. Last national data available from WHO, report that prevalence of hypercholesterolemia (>5.0 mmol/L) in Mozambique was 25.2% in males and 24.9% in females in 2008 [10]. At the moment, insufficient data are available about the epidemiology of hypercholesterolemia in Mozambique. Our study aims at describing the prevalence of hypercholesterolemia in patients diagnosed with diabetes and hypertensionand investigate possible risk factors to identify specific risk groups.
Study design and setting: we conducted a cross-sectional study on electronic medical records (EMR) of the Zimpeto DREAM Centre in Maputo, Mozambique. The Community of Sant´Egidio runs the Zimpeto Health Centre within the DREAM program and it was established in June 2018. The DREAM program is a public health program active in several African countries providing some health services: HIV care, TB treatment, HPV screening and treatment, hypertension and diabetes prevention and treatment [11-15].
Study population: we included all the patients diagnosed with hypertension and/or diabetes in the facility. In Zimpeto DREAM Centres all the patients are screened for diabetes and hypertension and if diagnosed, are followed up. In the present analysis we included all consecutive patients accessing the centre meeting the inclusion criteria. The inclusion criteria was: being diagnosed with diabetes and/or hypertension and undergo a full evaluation for non-communicable diseases from the beginning of the activities of the centre, up to the end of November 2020. Exclusion criteria were: age <18 years and pregnancy or breastfeeding.
Data collection and definitions: for each patient, anthropometric, clinical and laboratory data were collected. Hypertension and diabetes were diagnosed according to national guidelines. The better reference level for waist circumference (WC) in African population is under debate [16,17]. In absence of clear evidences, we followed the international standards, and we defined increased WC as WC >94cm in men and WC >80cm in women [18]. Hypertension was defined as blood pressure (BP) higher than 140 mmHg or 90 mmHg at three measurements [19]; diabetes was diagnosed if fasting blood glucose was higher than 126 mg/dL [20]. Hypercholesterolemia was defined as total blood cholesterol >200 mg/dL [1].
Statistical analysis: statistical data analysis was performed using SPSS 21 software (IBM Corp., Armonk, NY). Variables are presented as median with interquartile range (IQR). Crude and adjusted odds ratios (cOR and aOR) are reported with 95% confidence interval (CI). Chi-square test was used for the univariable analysis of factors associated with hypercholesterolemia. We included in the multivariable logistic regression all the variables that resulted in being associated with hypercholesterolemia at the univariable analysisat a 0.2 significance threshold.
Ethical considerations: all the services in the site of the study are delivered in collaboration and agreement with the local and national health authorities. The study used only clinical routine data collected during the service delivery andall the data were anonymized before extraction. For these reasons the study was exempted from specific consent.
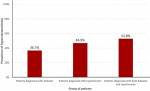
On the whole, 885 patients were included; 76.2% (n=674) were female. The characteristics of the cohort are shown in Table 1. Hypertension alone was diagnosed in 670 (75.7%) patients, diabetes in 109 (12.3%) patients and 106 (11.9%) patients were diagnosed with both hypertension and diabetes. Among the 885 patients enrolled, 410 (46.3%) patients had hypecholesterolemia. Figure 1 shows the rate of hypercholesterolemia among the patients diagnosed with diabetes, hypertension or both. Hypercholesterolemia was more prevalent in patients diagnosed with both diabetes and hypertension (52.8%), as compared to the patients diagnosed with hypertension (46.9%) or diabetes alone (36.7%).
Table 2 shows the results of the univariable and multivariable analysis. In the univariable analysis, the factors significantly associated with hypercholesterolemia were female sex, a body mass index (BMI) >25kg/m2 and being diagnosed with hypertension. However, in the multivariable analysis, only female sex (aOR 1.77, 95% CI 1.26-2.48, p=0.001) and BMI >25kg/m2 (aOR 1.50, 95% CI 1.11-2.04, p=0.008) were independently associated with increased hypercholesterolemia.
To our knowledge, our study is the first attempt to assess the prevalence of hypercholesterolemia in a population of patients accessing a health facility in Mozambique. In our cohort, 46.3% of patients presented hypercholesterolemia. It is worth to notice that these patients accessed the centre for other reasons and were subsequently diagnosed with hypertension and diabetes. Hypercholesterolemia was only a secondary diagnosis. The prevalence was even higher (52.8%) if considering patients diagnosed with both hypertension and diabetes. If other studies would confirm these data, a more systematic screening for hypercholesterolemia should be implemented in Mozambique for patients accessing health care for hypertension and/or diabetes.
The extensive review by Noubiap and colleagues involving 177 studies from several African countries (but not Mozambique), reported a pooled prevalence of hypercholesterolemia in patients with diabetes and hypertensionslightly lower than ours (respectively 38.0% and 34.4%). However, the trend is similar. Our results can highlight the hidden burden of dyslipidemia on patients accessing health care also in Mozambique. Blood cholesterol is not routinely assessed in many African countries and our results strengthen the advice for a full evaluation of patients even in African health facilities. Moreover, our data reported hypercholesterolemia as an independent condition, as it was independently associated only with female sex and increased BMI. Our cohort was disproportionally composed of women (76,2%). This finding is in line with the so called “gender paradox” and the lower rate of males seeking for care in comparison to women observed in many context [21,22].
The association with increased BMI was also described in other settings [23]. Interestingly, our results did not find any association between waist circumference and hypercholesterolemia. Although some studies found associations between central obesity and hypercholesterolemia, scholars are not unanimous about what is the best obesity index to correlate with metabolic disorders [23,24]. In our cohort, BMI was the only factor associated with hypercholesterolemia. The association with female sex is in line with data described in other African countries [25,26]. Similarly, the WHO reports that 11% of male and 24% of females are obese or overweight in Mozambique [6].
We are aware of some limitations of the present study. The absence of more detailed information about the cohort. Some critical information about other cardiovascular risk factors (such as familiarity, physical activity, tobacco and alcohol consumption) and lipidic asset (high-density lipoprotein (HDL), low-density lipoprotein (LDL) and triglyceride) were lacking. Notwithstanding these limitations, the main strength of our analysis is that it is based on field data, similar to the information that physician could access in everyday activity. In this perspective, our results strengthen the need for special attention to pay to particular groups of patients at higher risk for concomitant hypercholesterolemia.
This study shows that about half of patients diagnosed with hypertension and diabetes had concomitant hypercholesterolemia. Independent factors associated with hypercholesterolemia included were female sex and being overweight. Consequently, our results suggest the need for a more specific focus on female and obese/overweight patients, especially if diagnosed with both hypertension and diabetes, to promptly detect metabolic disorders and establish temporary preventive measures for cardiovascular events.
What is known about this topic
- Hypercholesterolemia is a prevalent health challenge in African countries burdening around 25.5% of the adult population;
- Hypercholesterolemia is strongly associated with other NCDs and mortality.
What this study adds
- We found that a high proportion of patients diagnosed with diabetes and hypertension (46.3%) are concomitantly affected with hypercholesterolemia;
- Our study found that in Mozambican patients with diabetes and hypertension, hypercholesterolemia is an independent condition, associated with female sex and increased BMI;
- Hypercholesterolemia is present in up to 52.8% of patients, we suggest the need for a more accurate and broader NCD screening in chronic patients in Mozambique.
The authors declare no competing interests.
FC conceived the study, analyzed data and drafted the manuscript; NM supervised data collection and revised the drafts; SP supervised data interpretation and revised the final version of the manuscript; MA and CM collected the data; SO and GG interpreted data and revised the drafts; PS interpreted data and supervised the manuscript drafting; MCM conceived the study and revised the final version of the manuscript. All the authors have read and agreed to the final mansucript.
Table 1: characteristics of the cohort
Table 2: factors associated with hypercholesterolemia in univariable and multivariable analysis
Figure 1: prevalence of hypercholesterolemia in patients with hypertension, diabetes, or both
- World Health Organization. Mean cholesterol - global health observatory (GHO) data. 2020.
- Noubiap JJ, Bigna JJ, Nansseu JR, Nyaga UF, Balti EV, Echouffo-Tcheugui JB et al. Prevalence of dyslipidaemia among adults in Africa: a systematic review and meta-analysis. Lancet Glob Health. 2018;6(9):e998-e1007. PubMed | Google Scholar
- Haregu TN, Byrnes A, Singh K, Sathish T, Pasricha N, Wickramasinghe K et al. A scoping review of non-communicable disease research capacity strengthening initiatives in low and middle-income countries. Glob Health Res Policy. 2019;4:31. PubMed | Google Scholar
- Kassa M, Grace J. The global burden and perspectives on non-communicable diseases (NCDs) and the prevention, data availability and systems approach of NCDs in low-resource countries. Public Health in Developing Countries-Challenges and Opportunities: IntechOpen. 2019. Google Scholar
- Gouda HN, Charlson F, Sorsdahl K, Ahmadzada S, Ferrari AJ, Erskine H et al. Burden of non-communicable diseases in sub-Saharan Africa, 1990-2017: results from the global burden of disease study 2017. Lancet Glob Health. 2019;7(10):e1375-e87. PubMed | Google Scholar
- World Health Organization. Noncommunicable diseases country profiles 2018. 2018. Google Scholar
- Amuyunzu-Nyamongo M, Owuor JO, Blanchard C. The consortium for NCD prevention and control in sub-Saharan Africa (CNCD-Africa): from concept to practice. Glob Health Promot. 2013;20(4 Suppl):97-103. PubMed | Google Scholar
- McQueen D, Pratt M, Blanchard C. Commentary on a meeting entitled 'building global capacity for non-communicable diseases (NCD) prevention: defining direction and roles'. Glob Health Promot. 2013;20(4_suppl):93-6. PubMed | Google Scholar
- Ciccacci F, Orlando S, Majid N, Marazzi C. Epidemiological transition and double burden of diseases in low-income countries: the case of Mozambique. The Pan African Medical Journal. 2020;37:49. PubMed | Google Scholar
- World Health Organization. Raised total cholesterol (>= 5.0 mmol/L) (crude estimate) - the global health observatory. 2020.
- Ciccacci F, Tolno VT, Doro Altan AM, Liotta G, Orlando S, Mancinelli S et al. Noncommunicable diseases burden and risk factors in a cohort of HIV+ elderly patients in Malawi. AIDS Res Hum Retroviruses. 2019;35(11-12):1106-1111. PubMed | Google Scholar
- Floridia M, Ciccacci F, Andreotti M, Hassane A, Sidumo Z, Magid NA et al. Tuberculosis case finding with combined rapid point-of-care assays (Xpert MTB/RIF and Determine TB LAM) in HIV-positive individuals starting antiretroviral therapy in Mozambique. Clin Infect Dis. 2017;65(11):1878-83. PubMed | Google Scholar
- Liotta G, Marazzi MC, Mothibi KE, Zimba I, Amangoua EE, Bonje EK et al. Elimination of mother-to-child transmission of HIV infection: the drug resource enhancement against AIDS and malnutrition model. Int J Environ Res Public Health. 2015;12(10):13224-39. PubMed | Google Scholar
- Magnano San Lio M, Mancinelli S, Palombi L, Buonomo E, Altan AD, Germano P et al. The DREAM model's effectiveness in health promotion of AIDS patients in Africa. Health Promot Int. 2009;24(1):6-15. PubMed | Google Scholar
- Palombi L, Pirillo MF, Andreotti M, Liotta G, Erba F, Sagno JB et al. Antiretroviral prophylaxis for breastfeeding transmission in Malawi: drug concentrations, virological efficacy and safety. Antivir Ther. 2012;17(8):1511-9. PubMed | Google Scholar
- Ekoru K, Murphy G, Young E, Delisle H, Jerome C, Assah F et al. Deriving an optimal threshold of waist circumference for detecting cardiometabolic risk in sub-Saharan Africa. Int J Obes (Lond). 2018;42(3):487-94. PubMed | Google Scholar
- Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. 2020;16(3):177-189. PubMed | Google Scholar
- World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 8-11 December 2008. 2011. Google Scholar
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-104. PubMed | Google Scholar
- Alberti G, Zimmet P, Shaw J, Grundy SM. The IDF consensus worldwide definition of the metabolic syndrome. Brussels: International Diabetes Federation. 2006;23(5):469-80.
- Alberts SC, Archie EA, Gesquiere LR, Altmann J, Vaupel JW, Christensen K. The male-female health-survival paradox: a comparative perspective on sex differences in aging and mortality. Sociality, hierarchy, health: comparative biodemography: a collection of papers: National Academies Press (US). 2014. Google Scholar
- Baker P, Shand T. Men's health: time for a new approach to policy and practice. J Glob Health. 2017;7(1):010306. PubMed | Google Scholar
- Bogers RP, Bemelmans WJE, Hoogenveen RT, Boshuizen HC, Woodward M, Knekt P et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167(16):1720-8. PubMed | Google Scholar
- Abbasi F, Blasey C, Reaven GM. Cardiometabolic risk factors and obesity: does it matter whether BMI or waist circumference is the index of obesity. Am J Clin Nutr. 2013;98(3):637-40. PubMed | Google Scholar
- Reiger S, Jardim TV, Abrahams-Gessel S, Crowther NJ, Wade A, Gomez-Olive FX et al. Awareness, treatment and control of dyslipidemia in rural South Africa: the HAALSI (health and aging in Africa: a longitudinal study of an INDEPTH community in South Africa) study. PloS one. 2017;12(10):e0187347. PubMed | Google Scholar
- Lyons JG, Sliwa K, Carrington MJ, Raal F, Pretorius S, Thienemann F et al. Lower levels of high-density lipoprotein cholesterol in urban Africans presenting with communicable versus non-communicable forms of heart disease: the 'Heart of Soweto' hospital registry study. BMJ Open. 2014;4(7):e005069. PubMed | Google Scholar