Emergency department utilization for sickle cell disease in St. Vincent and the Grenadines
Shelly-Ann Williams, Shakel Henson, Shenese Trimmingham, Jill Newman, Julie Kanter
Corresponding author: Shelly-Ann Williams, Department of Pediatrics, Medical University of South Carolina, Charleston, South Carolina, United States of America 
Received: 14 Dec 2020 - Accepted: 11 Jan 2021 - Published: 29 Jan 2021
Domain: Non-Communicable diseases epidemiology,Urgent Care Medicine,Pediatric hematology
Keywords: Sickle cell disease, St. Vincent, Grenadines, diagnosis, emergency service, emergency department
©Shelly-Ann Williams et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Shelly-Ann Williams et al. Emergency department utilization for sickle cell disease in St. Vincent and the Grenadines. Pan African Medical Journal. 2021;38:100. [doi: 10.11604/pamj.2021.38.100.27424]
Available online at: https://www.panafrican-med-journal.com//content/article/38/100/full
Emergency department utilization for sickle cell disease in St. Vincent and the Grenadines
Shelly-Ann Williams1,&, ![]() Shakel Henson2, Shenese Trimmingham2, Jill Newman1,
Shakel Henson2, Shenese Trimmingham2, Jill Newman1, ![]() Julie Kanter3
Julie Kanter3
&Corresponding author
Introduction: sickle cell disease (SCD) is a chronic illness. Individuals affected by this disease are at risk for lifelong complications including episodes of acute pain, chronic pain and multi-organ injury that leads to reduced quality of life and a shortened life span. There is a wealth of data on acute care utilization for SCD in the United States. However, data from the Caribbean region is limited. The objective of this study is to explore Emergency Department (ED) utilization for SCD in St. Vincent and the Grenadines by describing: i) the characteristics of SCD related ED encounters; ii) the urgency of these encounters as defined by resource utilization; iii) the disposition for these ED encounters.
Methods: the study was a cross-sectional study utilizing data from the ED log books at the Milton Cato Memorial Hospital (MCMH) during non-consecutive time periods between January 1st, 2012 - December 31st, 2016.
Results: there were 666 SCD-related ED encounters during the study period. Thirty-four percent of encounters resulted in hospitalization and 66% of encounters met criteria for an urgent visit. The most commonly reported diagnosis was vaso-occlusive crisis and accounted for 84% of all encounters. The most frequently documented age group was the 18-30 age category at 43%.
Conclusion: although SCD comprised less than 2% of all ED visits, the majority of these visits could be classified as urgent visits based on resource utilization. This study adds to the emerging data on the burden of this disease in this St. Vincent and the Grenadines.
Sickle cell disease (SCD) is a chronic illness that is caused by a mutation in the beta globin chain of the hemoglobin molecule [1]. Individuals affected by this disease are at risk for long life complications including episodes of acute pain, chronic pain and multi-organ injury that leads to reduced quality of life and a shortened life span [1,2]. Studies from the United States (US) have shown that individuals with SCD have high rates of acute care utilization [3,4]. Data have also shown that individuals >18 years of age and uninsured or publicly insured have the highest acute care utilization rates [3,5,6]. In the absence of national SCD registries, it can be difficult to describe the burden of disease in populations. As such, researchers have relied on other approaches such as healthcare utilization data to help in identifying the needs of individuals with SCD [6]. Although there are concerns that high utilization rates may be due to inappropriate use of acute care services, some data support that these high rates may not be preventable and may in-fact be due to the severity of the illness [7,8]. Therefore, emergency department (ED) utilization studies may still be able to provide meaningful data regarding the burden of disease in populations. There is a wealth of data on acute care utilization for SCD in the US. However, data from the Caribbean region is limited. This study aims to evaluate ED use for SCD in St. Vincent and the Grenadines. St. Vincent and the Grenadines is a multi-island nation in the Caribbean where it is estimated that 1 in 172 newborns may be affected by SCD [9,10]. The objective of this study is to explore emergency department (ED) utilization for SCD in St. Vincent and the Grenadines by describing; i) the characteristics of SCD related ED encounters; ii) the urgency of these encounters as defined by resource utilization; iii) the disposition for these ED encounters.
Data source: the study was a cross-sectional study utilizing data from the ED log books at the Milton Cato Memorial Hospital (MCMH). Milton Cato Memorial Hospital was the country´s only public secondary referral hospital during the study period. At present, there is no computerized database of ED encounters at this hospital. Instead, there are hand-written logbooks that detail all ED encounters. For each ED encounter, the patient´s name, sex, age (but not date of birth), address, diagnoses, interventions performed during the encounter and final disposition are entered into logbooks. These logbooks provided the data for this study.
Study period and study population: the initial plan was to review all consecutive ED encounters from January 1st, 2012 - December 31st, 2016 and extract all SCD-related encounters. However, not all logbooks for this time period could be located. As a result, the data was limited to the non-consecutive block periods of 1/19/2012 - 5/14/2012, 9/14/2013 - 12/31/2013, 1/1/2014 - 3/31/2014, 1/10/2015 - 12/31/2015 and 1/1/2016 - 1/28/2016. All ED encounters for the time periods that were available were manually reviewed and SCD-related encounters were extracted. As there are no ICD codes documented in this logbook, all encounters with SCD or a SCD-related diagnosis were manually extracted and classified using the following criteria.
A confirmed SCD related encounter was defined as: i) an encounter that included documentation of SCD in the list of diagnoses OR; ii) an encounter with a SCD specific diagnosis (acute chest syndrome, vaso-occlusive crisis) without a documentation of SCD.
A possible SCD related encounter was defined as: an encounter that included an implied diagnosis, without a documentation of SCD (e.g. pain crisis, ''in crisis''), confirmed and possible SCD related encounters were included in the final analyses.
Variables: for eligible encounters we collected patient age at time of encounter, address, sex, date of the encounter, diagnoses documented, interventions performed and the final disposition. Study data were extracted from the logbooks and managed using Research Electronic Data Capture (REDCAP) tools hosted at the Medical University of South Carolina [11]. Research electronic data capture (REDCAP) is a secure, web-based software platform designed to support data capture for research studies, providing: 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
Urgency determination: resource utilization has been used in pediatric literature to determine the urgency of an ED encounter. Previous studies have defined an urgent ED encounter as any encounter that i) results in an admission or ii) required an ED based service such as a laboratory test, a radiographic study, an electrocardiogram or an echocardiogram [7,12,13]. Echocardiography was not available at this institution during the study period. Therefore, for this study, we defined an urgent encounter as any ED encounter that resulted in an admission OR a ''treat and release'' encounter that included any laboratory testing or any radiographic study.
Statistical analysis and outcomes: descriptive analyses were performed using the SAS version 9.4 (Cary, USA). Frequencies and proportions were used to describe study demographics, population clinical characteristics and diagnoses. Diagnoses, encounter classifications and encounter dispositions were further analyzed by age groups and reported as frequencies and percentages.
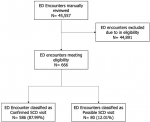
During the periods for which data were available, there were a total of 45,557 visits to the ED. Of these 666 (1.46%) met eligibility criteria and were included in the final analysis. Eighty-eight percent were classified as confirmed SCD-related encounters and 12% were classified as a possible SCD-related encounter (Figure 1). Patient and ED encounters are summarized in (Table 1). Sixty-seven percent of the encounters were by female patients. The age 18-30 category had the most frequent encounters at 42.94% followed by the age category of 10-17 at 20.42%. Among the diagnoses, vaso-occlusive crisis (VOC) was the most commonly recorded diagnosis at 83.63%. Acute chest syndrome (7.36%) and acute viral illness (3.30%) were the second and third most commonly recorded diagnosis respectively. Thirty-four percent of encounters resulted in hospitalization and 66% of encounters met criteria for an urgent visit. Table 2 stratifies diagnoses by age. Across all age groups, VOC was the most commonly recorded diagnosis. Although there were some differences in the second and third most commonly recorded diagnosis among the different groups, lung conditions in the form of either acute chest syndrome or pneumonia/lower respiratory tract infections were in the top three most commonly reported diagnoses across all age groups. Encounter classification and disposition were also evaluated and stratified by age and are summarized in (Table 3, Table 4). For all age groups, the majority of encounters were classified as an urgent visit.
This study utilized available national level data to describe ED utilization for SCD in St. Vincent and the Grenadines. Results of this study showed that less than 2% of all ED encounters were SCD related encounters. However, the majority of encounters could be classified as urgent visits. Similar to other published literature, VOC accounted for the majority of SCD-related encounters [14-16]. When stratified by age, VOC still remained the most common diagnosis. The most frequently documented age group was the 18-30 age category, which is also similar to data from Schlenz et al. [6]. About 1/3 of all encounters resulted in an admission, which is similar to other studies that showed admission rates of around 29% [14]. Although for all age groups most encounters resulted in discharge, when looked at using resource utilization, most encounters were classified as urgent encounters. To our knowledge, this the first study that examines ED utilization on a national level for St. Vincent and the Grenadines. This study therefore provides valuable insight that will likely benefit health officials and health care providers in St. Vincent and the Grenadines. This study has several limitations. First, we were unable to identify unique individuals given the limitations of the data that are stored in the logbooks. As a result, we were not able to provide data on acute care utilization rates per individual.
Data have shown that in any given year, 50-60% of persons with SCD have no ED visits but that 20% of patients will have 3 or more acute care encounters per year [3,4,17]. Therefore, it is possible that there may have been a small subset of ''high utilizers'' that may be driving the results of this study. Nevertheless, this study is the first to provide national estimates for ED utilization for SCD in St. Vincent and the Grenadines. Since ED services are publicly funded in this population, these data will be very beneficial and informative to local health officials. The second major limitation was that many of the logbooks could not be located. As such, our data was limited to non-consecutive time periods between January 1st, 2012 to December 31st, 2016. It is possible that this could have affected the results of our study. However, the missing logbooks would have included all ED visits for those missing time periods. Therefore, non SCD-related encounters would have been missing as well. Given the number of SCD related encounters (n=666) that were available for analysis, we believe that this is a large enough sample size to provide meaningful results. Third, it was not always possible to determine the primary diagnosis for the encounters based on the information that was entered into the logbooks. It is possible that in some cases, SCD was a secondary diagnosis and not related to the reason for the visit. Nonetheless, our results revealed that VOC crisis was the most commonly documented diagnosis. This is in keeping with other published data suggesting that we were still able to provide a reasonable description of ED utilization for SCD in this population [14,15,18]. Finally, the total population of individuals living with SCD in this country is not known. Thus, it is unclear the percentage of individuals that visit the ED. Future studies should be conducted that address utilization at the individual level.
Individuals with SCD utilize the ED for a variety of reasons. The most frequently documented diagnosis was VOC, and the age group 18-30 was the most commonly documented age group. Although SCD comprised less than 2% of all ED visits, the majority of these visits could be classified as urgent visits based on resource utilization. This study adds to the emerging data on the burden of this disease in this St. Vincent and the Grenadines. It will likely inform local providers and policy makers on the ED utilization for SCD and can lead to improvements in care provided to individuals with SCD in the future.
What is known about this topic
- Individuals with sickle cell disease have high acute care utilization rates sickle cell disease;
- Data from US shows that adults >18 years of age or uninsured show highest acute care utilization rates.
What this study adds
- There is currently limited data on acute care utilization for sickle cell disease in the Caribbean;
- This is the first study to evaluate acute care utilization for sickle cell disease in St. Vincent and the Grenadines.
The authors declare no competing interests.
Shelly-Ann Williams contributed to research design, data collection, manuscript preparation, participated in the revision process and gave final approval of the version submitted. Shakel Henson contributed to data collection, manuscript preparation, participated in the revision process and gave final approval of the version submitted. Shenese Trimmingham contributed to data collection, was part of the manuscript review process and gave final approval of the version submitted. Jill Newman contributed to data analysis, the manuscript review and revision process and gave final approval of the version submitted. Julie Kanter contributed to research design, the manuscript review and revision process and gave final approval of the version submitted. All the authors have read and agreed to the final manuscript.
We would like to thank the Ministry of Health, Wellness and the Environment of St. Vincent and the Grenadines and the administrative staff of the Milton Cato Memorial Hospital.
Table 1: characteristics of ED encounters for SCD from 2012-2016 (n=666)
Table 2: diagnoses by age groups (n=666)
Table 3: encounter classification by age groups (n=666)
Table 4: encounter disposition by age groups (n=666)
Figure 1: flow diagram of study population
- Kanter J, Kruse-Jarres R. Management of sickle cell disease from childhood through adulthood. Blood Rev. 2013 Nov;27(6):279-87. PubMed | Google Scholar
- McCavit TL. Sickle cell disease. Pediatr Rev. 2012;33(5):195-204;205-206. PubMed | Google Scholar
- Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288-1294. PubMed | Google Scholar
- Shankar SM, Arbogast PG, Mitchel E, Cooper WO, Wang WC, Griffin MR. Medical care utilization and mortality in sickle cell disease: a population-based study. Am J Hematol. 2005;80(4):262-270. PubMed | Google Scholar
- Panepinto JA, Owens PL, Mosso AL, Steiner CA, Brousseau DC. Concentration of hospital care for acute sickle cell disease-related visits. Pediatr Blood Cancer. 2012 Oct;59(4):685-9. PubMed | Google Scholar
- Schlenz AM, Boan AD, Lackland DT, Adams RJ, Kanter J. Needs assessment for patients with sickle cell disease in South Carolina, 2012. Public Health Rep. Jan-Feb 2016;131(1):108-16. PubMed | Google Scholar
- Bundy DG, Strouse JJ, Casella JF, Miller MR. Urgency of emergency department visits by children with sickle cell disease: a comparison of 3 chronic conditions. Acad Pediatr. Jul-Aug 2011;11(4):333-41. PubMed | Google Scholar
- Nimmer M, Hoffmann RG, Dasgupta M, Panepinto J, Brousseau DC. The proportion of potentially preventable emergency department visits by patients with sickle cell disease. J Pediatr Hematol Oncol. 2015 Jan;37(1):48-53. PubMed | Google Scholar
- Pan American health organization, World health organization (WHO). Health in the Americas: regional outlook and country profiles. Washington DC, PAHO. 2017.
- Williams SA, Browne B, Reed S, Taylor S, Summer A, Kanter J. Prevalence of sickle cell disease among newborns in St. Vincent and the Grenadines: a retrospective study. West Indian Med J. 2017;66(4):486-490. Google Scholar
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81. PubMed | Google Scholar
- Brousseau DC, Hoffmann RG, Nattinger AB, Flores G, Zhang Y, Gorelick M. Quality of primary care and subsequent pediatric emergency department utilization. Pediatrics. 2007;119(6):1131-1138. PubMed | Google Scholar
- Mistry RD, Hoffmann RG, Yauck JS, Brousseau DC. Association between parental and childhood emergency department utilization. Pediatrics. 2005 Feb;115(2):e147-51. PubMed | Google Scholar
- Yusuf HR, Atrash HK, Grosse SD, Parker CS, Grant AM. Emergency department visits made by patients with sickle cell disease: a descriptive study, 1999-2007. Am J Prev Med. 2010;38(4):536-541. PubMed | Google Scholar
- Lanzkron S, Carroll CP, Haywood C. The burden of emergency department use for sickle-cell disease: an analysis of the national emergency department sample database. Am J Hematol. 2010 Oct;85(10):797-9. PubMed | Google Scholar
- Panepinto JA, Brousseau DC, Hillery CA, Scott JP. Variation in hospitalizations and hospital length of stay in children with vaso-occlusive crises in sickle cell disease. Pediatr Blood Cancer. 2005 Feb;44(2):182-6. PubMed | Google Scholar
- Yang YM, Shah AK, Watson M, Mankad VN. Comparison of costs to the health sector of comprehensive and episodic health care for sickle cell disease patients. Public Health Rep. Jan-Feb 1995;110(1):80-6. PubMed | Google Scholar
- Galloway-Blake K, Reid M, Walters C, Jaggon J, Lee MG. Clinical factors associated with morbidity and mortality in patients admitted with sickle cell ddisease. West Indian Med J. 2014 Dec;63(7):711-6. PubMed | Google Scholar