Prevalence and correlates of multiple non-communicable disease risk factors among adults in Zambia: results of the first national STEPS survey in 2017
Supa Pengpid, Karl Peltzer
Corresponding author: Karl Peltzer, Department of Research Administration and Development, University of Limpopo, Polokwane, South Africa 
Received: 17 Jul 2020 - Accepted: 14 Nov 2020 - Published: 24 Nov 2020
Domain: Chronic disease prevention,Public health
Keywords: Risk factors, non-communicable diseases, prevalence, adults, Zambia
©Supa Pengpid et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Supa Pengpid et al. Prevalence and correlates of multiple non-communicable disease risk factors among adults in Zambia: results of the first national STEPS survey in 2017. Pan African Medical Journal. 2020;37:265. [doi: 10.11604/pamj.2020.37.265.25038]
Available online at: https://www.panafrican-med-journal.com//content/article/37/265/full
Research 
Prevalence and correlates of multiple non-communicable disease risk factors among adults in Zambia: results of the first national STEPS survey in 2017
Prevalence and correlates of multiple non-communicable disease risk factors among adults in Zambia: results of the first national STEPS survey in 2017
Supa Pengpid1,2, Karl Peltzer2,&
&Corresponding author
Introduction: the prevalence of Non-Communicable Diseases (NCDs) is increasing in African countries. This study aimed to estimate the prevalence and correlates of multiple NCD risk factors (NCDRF) among the adult population in Zambia.
Methods: nationally representative cross-sectional data from 4,302 individuals aged 18-69 years of the “2017 Zambia STEPS survey” were analysed.
Results: the prevalence of insufficient fruit and vegetable consumption was 90.4%, followed by overweight/obesity (24.4%), low physical activity (19.5%), hypertension (18.9%), daily tobacco use (10.7%), sedentary behaviour (8.9%), suicidal behaviour (8.5%), alcohol dependence (7.4%), raised total cholesterol (7.4%), and diabetes (6.2%). The distribution of NCDRF was 41.5% 0-1 NCDRF, 48.2% 2-3, 10.4% 4-10, and 26.7% 3-10 NCDRF. In adjusted ordinal logistic regression analysis, compared to persons aged 18-34 years, individuals aged 50-69 years were 3.58 times (AOR: 3.58, 95% CI: 3.95-4.49) more likely to have a higher number of NCDRF. Women were 24% (AOR: 1.24, 95% CI: 1.03-1.49) more likely than men to have a higher number of NCDRF. Persons living in urban locations were 71% (AOR: 1.74, 95% CI: 1.43-2.16) more likely than persons living in rural locations to have a higher number of NCDRF, and compared to individuals with lower than primary education, persons with more than primary education were 20% (AOR: 0.80, 95% CI: 0.65-0.98) less likely to have a higher number of NCDRF.
Conclusion: more than one in four study participants had three to ten NCDRF and several associated factors were found that can aid to target interventions.
In Zambia 29% of mortality was attributed to non-communicable diseases (NCDs) in 2016 [1]. A high proportion (>80%) of premature deaths from NCDs, such as cardiovascular diseases, diabetes, cancer, and respiratory diseases, occur in low- and middle-income countries [2]. Major behavioural NCD risk factors (NCDRF) increasing the risk of NCD death include tobacco use, unhealthy diet, low physical activity, and hazardous and harmful alcohol use [2]. Considering the increasing trend of NCDs in Africa, it is “crucial to have a careful understanding of the local drivers of NCDs” [3]. Against this backdrop, national data on NCDRF are needed in a lower-middle income Southern African country, Zambia. Some studies in Zambia were subnational (Lusaka urban district) and only focused on specific NCDRF, such as high cholesterol levels (15.8%) [4], obesity (14.2%) [5], diabetes (4.0%) [6] and hypertension (34.8%) [7]. In two rural districts (Kaoma and Kasama) in Zambia, the prevalence of hypertension was 25.8% and 30.3%, respectively [8]. The adult prevalence of diabetes of 3.5% was found in a household survey in five of ten provinces in 2010 in Zambia [9].
In previous national STEPS surveys in three African countries and in Nepal, the prevalence of multiple NCDRF was as follows: 75.8% 4-12 NCDRF (18-69 years in 2015) in Kenya [10], 16.5% 3-7 NCDRF (24-64 years in 2009) in Malawi [11], 17.3% 3-5 NCDRF (18-69 years in 2014) in Uganda [12], and 27.7% 3-8 NCDRF (15-69 years in 2013) in Nepal [13]. Table 1 shows the distribution of individual NCDRF in Kenya, Malawi, Uganda, and Nepal [10-17]. Regarding biological NCDRF, the prevalence of raised total cholesterol ranged from 6.7% in Uganda to 22.6% in Nepal, raised blood ranged from 1.4% in Uganda to 5.6% in Malawi, hypertension ranged from 23.8% in Kenya to 32.0% in Malawi, and general overweight/obesity ranged from 18.1% in Malawi to 27.9% in Kenya. In terms of behavioural NCDRF, the prevalence of inadequate fruit and vegetable intake ranged from 87.8% in Uganda to 98.9% in Nepal, current tobacco smoking ranged from 9.6% in Uganda to 18.5% in Nepal, low physical activity ranged from 3.4% in Nepal to 9.5% in Malawi, and harmful alcohol use (heavy episodic drinking) ranged from 2.0% in Nepal to 16.7% in Uganda (Table 1).
Factors associated with a higher number of biological and behavioural NCDRF include increasing age [10,13,18-20], women [10], men [13,18], currently married [13], ecological zone [13] or region [12], lower education [13], higher education [18], geolocality [12], higher socioeconomic status [18, 20], and residing in urban areas [18,20]. The study aimed to assess the prevalence and correlates of NCDRF among individuals aged 18-69 years in Zambia.
Nationally representative cross-sectional data from the “2017 Zambia STEPS Survey” were analysed [21]. A “multi-stage cluster sampling technique was used to select a nationally representative sample of adults in Zambia aged 18 to 69 years.” [22]. “In the first stage of sampling, Standard Enumeration Areas (SEAs) were selected from each province using a probability proportional to size (PPS), and in the second stage, 15 households in rural SEAs and 20 households in urban SEAs were selected systematically using an appropriate sampling interval based on the number of households in that SEA.”[22]. More information on the sampling strategy and the 2017 Zambia STEPS survey data can be publicly accessed; the survey response rate was 74.3%.” [22]. “The study was approved by the University of Zambia (UNZA) Research Ethics Committee (REC), and written informed consent was obtained from participants.” [22].
Measures
NCD outcome variables: biological NCDRF. Diabetes was classified as “fasting plasma glucose levels =7.0 mmol/L, and/or currently taking insulin or oral hypoglycemic drugs”; raised total cholesterol (TC) as “fasting TC =5.0 mmol/L or currently on medication for raised cholesterol”; hypertension as “systolic BP =140 mm Hg and/or diastolic BP =90 mm Hg or currently on antihypertensive medication”; and measured Body Mass Index (”25-29.9 kg/m2 overweight and =30 kg/m2 obesity”) [22].
Behavioural NCDRF consisted of insufficient fruit and vegetable consumption (<5 servings/day), low physical activity, and sedentary behaviour (=8 hours/day) based on the “Global Physical Activity Questionnaire”, daily tobacco use, and alcohol dependence (defined as =4 scores on item 4-6 of the “Alcohol Use Disorder Identification Test=AUDIT” [22]. Suicidal behaviour was based on three questions on suicidal ideation, plans, and/or attempts in the past year [22]. Sociodemographic information included marital status, age, sex, highest educational level, work status, ethnic affiliation, and geolocality [22].
Data analysis: statistical procedures were done with “STATA software version 15.0 (Stata Corporation, College Station, Texas, USA),” taking the multistage sampling design and data weighting into account [22]. The total number of ten NCDRF were grouped into 1=0-1, 2=2-3, and 3=4-10 NCDRF and described with bar graphs and frequency tabulations. Unadjusted and adjusted ordinal logistic regressions were utilized to assess predictors of the number of NCDRF (0-1, 2-3, and 4-10). Co-variates were selected based on a previous literature review [10,13,18-20]. Only complete cases were included in the analysis, and p<0.05 was set as significant.
Characteristics of the sample and NCDRF: the study population included 4,302 individuals aged 18-69 years (31 years median age, IQR 23-41). Almost half of the study participants (48.7%) were men, 59.1% were married or cohabiting, 28.7% were unemployed, 71.1% had primary or more education, 32.8% were Bemba and 48.8% resided in urban areas. The prevalence distribution of individual biological NCDRF was 7.4% raised total cholesterol, 6.2% diabetes, 24.4% overweight/obesity, and 18.9% hypertension. The prevalence distribution of individual behavioural NCDRF was 90.4% insufficient fruit and vegetable consumption, 19.5% low physical activity, 10.7% daily tobacco use, 8.9% sedentary behaviour, 8.5% suicidal behaviour, and 7.4% alcohol dependence. The prevalence of overweight/obesity, low physical activity, raised total cholesterol, and suicidal behaviour was significantly higher in women than in men, and the prevalence of daily tobacco use and alcohol dependence was significantly higher in men than in women (Table 1, Table 2).
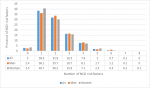
Frequency distribution of NCDRF: the prevalence of having no NCDRF was 3.0%, one 38.5%, two 31.9%, three 16.3%, four 7.6%, five 2.0%, six 0.7%, seven 0.1% and 8-10 risk factors zero percent (Figure 1). Overall, 41.5% of the participants had 0-1 NCD risk factor, 48.2% 2-3 risk factors, 10.4% 4-10, and 26.7% three or more NCDRF. A higher number of NCDRF increased with age, urban residence, and female sex, and among men who were never married, separated, divorced, or widowed (Table 3).
Associations with the number of NCDRF: Table 4 shows the univariate associations with NCDRF counts. In the adjusted ordinal logistic regression analysis, compared to persons aged 18-34 years, individuals aged 50-69 years were 3.58 times (AOR: 3.58, 95% CI: 3.95-4.49) more likely to have a higher number of NCDRF. Women were 24% (AOR: 1.24, 95% CI: 1.03-1.49) more likely than men to have a higher number of NCDRF. Persons living in urban locations were 71% (AOR: 1.74, 95% CI: 1.43-2.16) more likely than persons living in rural locations to have a higher number of NCDRF, and compared to individuals with lower than primary education, persons with more than primary education were 20% (AOR: 0.80, 95% CI: 0.65-0.98) less likely to have a higher number of NCDRF (Table 5).
The nationally representative 2017 Zambia STEPS survey among individuals aged 18-69 years found a high prevalence of 3-10 NCDRF (26.7%), which was similar to Nepal (27.7% 3-8 NCDRF [13], lower than in Kenya (75.8% 4-12 NCDRF [10], but higher than in Malawi (16.5% 3-7 NCDRF) [11], and Uganda (17.3% 3-5 NCDRF) [12]. The high clustering of NCDRF in this survey increases the risk of NCDs in the adult population in Zambia. Consistent with previous research [10,13-20], this survey found that increasing age, female sex, lower education, and urban residence were associated with a higher number of NCDRF. The promotion of early screening for NCDRF, targeting women, urban residents, and those with lower education, may help the prevention of the development of NCDs in Zambia. Unlike some previous research [13,20], this study did not find any significant association between marital status, employment status, ethnic group, and multiple NCDRF.
The four most prevalent individual NCDRF in this study were insufficient fruit and vegetable consumption (90.4%), overweight/obesity (24.4%), low physical activity (19.5%), and hypertension (18.9%). Similar proportions of individual NCD risk behaviours were found in the STEPS surveys in 2014 in Kenya [10] and in 2013 in Nepal [13]. The prevalence of hypertension (18.9%) in this study was lower than in previous local surveys in Zambia, 34.8% in the urban Lusaka district [7], and 25.5%-30.3% in two rural districts in Zambia [8]. The prevalence of overweight/obesity (24.4%) in this study was higher than in the urban Lusaka district study (14.2%) [5], and the prevalence of insufficient fruit/vegetable consumption (90.4%) was higher than in the 2003 Zambia World Health Survey (77.7%) [23], and the prevalence of low physical activity (19.5%) in this study was similar to data from the 2003 Zambia World Health Survey (23.3%) [23].
The prevalence of daily tobacco use (10.7%) and alcohol dependence (7.4%) in this survey was similar to the 2009 Malawi STEPS survey (14.1% smokers, and 7.7% excessive drinkers) [11,15], and the 2014 Kenya STEPS survey (10.1% smokers, and 12.7% harmful alcohol users) [10,14]. The proportions of daily tobacco use and alcohol dependence were similar to results from the 2003 Zambia World Health Survey (14.1% current smoking and 7.4% heavy episodic drinking) [23]. The increase of exercise taxes and prices on tobacco products and alcoholic beverages has been recommended in Zambia [22]. The prevalence of diabetes (6.2%) and raised total cholesterol (7.4%) in this study was similar to the 2009 Malawi STEPS survey (5.6% diabetes and 8.7% raised cholesterol) [11,15], but lower than in the 2014 Kenya STEPS survey in terms of high total cholesterol (10.1%), and higher in terms of diabetes (1.9%) [10,14]. Compared to the prevalence of raised total cholesterol (15.8%) in the Lusaka urban district STEPS survey [4], the prevalence of raised total cholesterol was lower in this study (7.4%), and the prevalence of diabetes (6.2%) was higher in this study than in the Lusaka urban district study (4.0%) [6], and the large community-based study in 2010 in Zambia (3.5%) [9].
Specific NCDRF differed by sex in this study, with substance being higher in men, and overweight/obesity, low physical activity, raised total cholesterol, and suicidal behaviour being higher in women. Similar sex differences in the prevalence of substance use, obesity, and raised total cholesterol were also found in the 2009 Malawi and 2014 Kenya STEPS surveys [10,11]. It is important to take these sex differences into account when designing NCD health promotion activities [11].
Study limitations include the cross-sectional design of the study, which prevents from causative inferences, and the questionnaire interview relying on self-report of the data. Some study variables, such as household income, could not be included in the analysis due to too many missing values.
In this national community-based 2017 STEPS survey among adults in Zambia, more than one in four study participants had three to ten NCDRF. Several factors associated with NCDRF counts were identified, including increasing age, female sex, residing in urban areas, and lower education that can be targeted in interventions to address multiple NCDRF in the Zambian population. Taking the clustering nature of NCDRF into account, interventions should be targeting multiple, in particular modifiable, NCDRF.
What is known about this topic
- Some subregional studies in Zambia report the prevalence of individual NCD risk factors;
- Some African countries report on the national prevalence of individual NCD risk factors;
- Some African countries, such as Kenya, Malawi, and Uganda, report on the national prevalence of multiple NCD risk factors.
What this study adds
- More than one in four persons in Zambia had three or more NCD risk factors;
- Older age, female sex, rural residence, and lower education increased the odds for an increasing number of NCD risk factors in the Zambian population;
- Taking the clustering nature of NCD risk factors into account, interventions should be targeting multiple, in particular modifiable, NCD risk factors.
The authors declare no competing interests.
All authors fulfil the criteria for authorship. SP and KP conceived and designed the research, performed statistical analysis, drafted the manuscript and made critical revision of the manuscript for key intellectual content. All authors read and approved the final version of the manuscript and have agreed to authorship and order of authorship for this manuscript.
The data source, the World Health Organization NCD Microdata Repository (URL: https://extranet.who.int/ncdsmicrodata/index.php/catalog), is hereby acknowledged.
Table 1: distribution of individual non-communicable diseases (NCDs) risk factors in four national STEPS surveys
Table 2: sample characteristics of survey participants aged 18-69 years in Zambia, 2017 (N=4302)
Table 3: distribution of non-communicable diseases (NCDs) risk factor counts among individuals 18-69 years in Zambia, 2017
Table 4: univariate ordinal logistic regression with non-communicable diseases risk factor counts among individuals aged 18-69 years in Zambia, 2017
Table 5: multivariable ordinal logistic regression with non-communicable diseases risk factor counts among individuals aged 18-69 years in Zambia, 2017
Figure 1: frequency of non-communicable diseases risk factors among adults in Zambia
- World Health Organization (WHO) Zambia. Noncommunicable Diseases (NCD) Country Profiles. 2018. Accessed on 14th June 2020.
- World Health Organization (WHO). Noncommunicable diseases. 2018. Accessed on 14th June 2020.
- Nyirenda MJ. Non-communicable diseases in sub-Saharan Africa: understanding the drivers of the epidemic to inform intervention strategies. Int Health. 2016;8(3):157-158. doi:10.1093/inthealth/ihw021. PubMed | Google Scholar
- Muula AS, Rudatsikira E, Babaniyi O, Songolo P, Mulenga D, Siziya S. Factors associated with high cholesterol levels in Lusaka, Zambia: A community-based study. Med J Zambia. 2012;39(4):12-7. PubMed | Google Scholar
- Rudatsikira E, Muula AS, Mulenga D, Siziya S. Prevalence and correlates of obesity among Lusaka residents, Zambia: a population-based survey. Int Arch Med. 2012;5(1):14. doi:10.1186/1755-7682-5-14. PubMed | Google Scholar
- Nsakashalo-Senkwe M, Siziya S, Goma FM, Songolo P, Mukonka V, Babaniyi O. Combined prevalence of impaired glucose level or diabetes and its correlates in Lusaka urban district, Zambia: a population based survey. Int Arch Med. 2011;4(1):2. Published 2011 Jan 12. doi:10.1186/1755-7682-4-2. PubMed | Google Scholar
- Goma FM, Nzala SH, Babaniyi O, Songolo P, Zyaambo C, Rudatsikira E et al. Prevalence of hypertension and its correlates in Lusaka urban district of Zambia: a population based survey. Int Arch Med. 2011;4:34. doi:10.1186/1755-7682-4-34. PubMed | Google Scholar
- Mulenga D, Siziya S, Rudatsikira E, Mukonka VM, Babaniyi O, Songolo P et al. District specific correlates for hypertension in Kaoma and Kasama rural districts of Zambia. Rural Remote Health. 2013;13(3):2345. PubMed | Google Scholar
- Bailey SL, Ayles H, Beyers N, Godfrey-Faussett P, Muyoyeta M, du Toit E, Yudkin JS, Floyd S. Diabetes mellitus in Zambia and the Western Cape province of South Africa: Prevalence, risk factors, diagnosis and management. Diabetes Res Clin Pract. 2016;118:1-11. doi: 10.1016/j.diabres.2016.05.001. PubMed | Google Scholar
- Wekesah FM, Nyanjau L, Kibachio J, Mutua MK, Mohamed SF, Grobbee DE et al. Individual and household level factors associated with presence of multiple non-communicable disease risk factors in Kenyan adults. BMC Public Health. 2018;18(Suppl 3):1220. doi:1186/s12889-018-6055-8. PubMed | Google Scholar
- Msyamboza KP, Ngwira B, Dzowela T, Msyamboza KP, Ngwira B, Dzowela T, Mvula C, Kathyola D, Harries AD et al. The burden of selected chronic non-communicable diseases and their risk factors in Malawi: nationwide STEPS survey. PLoS One. 2011;6(5):e20316. doi:10.1371/journal.pone.0020316. PubMed | Google Scholar
- Wesonga R, Guwatudde D, Bahendeka SK, Mutungi G, Nabugoomu F, Muwonge J. Burden of cumulative risk factors associated with non-communicable diseases among adults in Uganda: evidence from a national baseline survey. Int J Equity Health. 2016;15(1):195. doi:10.1186/s12939-016-0486-6. PubMed | Google Scholar
- Aryal KK, Mehata S, Neupane S, Vaidya A, Dhimal M, Dhakal P et al. The Burden and Determinants of Non Communicable Diseases Risk Factors in Nepal: Findings from a Nationwide STEPS Survey. PLoS One. 2015;10(8):e0134834. doi:10.1371/journal.pone.0134834. PubMed | Google Scholar
- World Health Organization (WHO). Non Communicable Diseases Risk Factors STEPS Survey Kenya 2015 Fact sheet . Accessed on 14th June 2020.
- World Health Organization (WHO). Malawi STEPS Survey 2009 Fact Sheet. Accessed on 14th June 2020.
- World Health Organization (WHO). Uganda STEPS Survey 2014 Fact Sheet. Accessed on 14th June 2020.
- World Health Organization (WHO). Non Communicable Diseases Risk Factors: STEPS Survey Nepal 2013 Factsheet. Accessed on 14th June 2020. PubMed | Google Scholar
- Zaman MM, Bhuiyan MR, Karim MN, MoniruzZaman, Rahman MM, Akanda AW et al. Clustering of non-communicable diseases risk factors in Bangladeshi adults: An analysis of STEPS survey 2013. BMC Public Health. 2015;15:659. doi:10.1186/s12889-015-1938-4. PubMed | Google Scholar
- Rafique I, Saqib MAN, Munir MA, Qureshi H, Rizwanullah, Khan SA et al. Prevalence of risk factors for noncommunicable diseases in adults: key findings from the Pakistan STEPS survey. East Mediterr Health J. 2018;24(1):33-41. PubMed | Google Scholar
- Pelzom D, Isaakidis P, Oo MM, Gurung MS, Yangchen P. Alarming prevalence and clustering of modifiable noncommunicable disease risk factors among adults in Bhutan: a nationwide cross-sectional community survey. BMC Public Health. 2017;17(1):975. doi:10.1186/s12889-017-4989-x. PubMed | Google Scholar
- World Health Organization (WHO). Noncommunicable diseases and their risk factors: STEPwise approach to surveillance (STEPS). 2018. Accessed on 14th June 2020.
- Republic of Zambia, Ministry of Health. Zambia STEPS for non-communicable disease risk factors. 2017. Accessed on 14th June 2020.
- Umuhoza SM, Ataguba JE. Inequalities in health and health risk factors in the Southern African Development Community: evidence from World Health Surveys. Int J Equity Health. 2018;17(1):52. doi:10.1186/s12939-018-0762-8. PubMed | Google Scholar