Presentation and anatomical distribution of diverticular disease in four hospitals in Sudan
Alsmwal Alnour Alnzaer, Ali Yasen Yasen Mohamedahmed, Yousif Abdalla Adam, Elmoiz Eltyiep, Suliman Hussen Suliman
Corresponding author: Ali Yasen Yasen Mohamedahmed, General Surgery, Sudan Medical Specialization Board, Khartoum, Sudan 
Received: 21 Apr 2020 - Accepted: 27 May 2020 - Published: 03 Jun 2020
Domain: General surgery
Keywords: Diverticular disease, rectal bleeding, constipation
©Alsmwal Alnour Alnzaer et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Alsmwal Alnour Alnzaer et al. Presentation and anatomical distribution of diverticular disease in four hospitals in Sudan. Pan African Medical Journal. 2020;36:64. [doi: 10.11604/pamj.2020.36.64.22987]
Available online at: https://www.panafrican-med-journal.com//content/article/36/64/full
Research 
Presentation and anatomical distribution of diverticular disease in four hospitals in Sudan
Presentation and anatomical distribution of diverticular disease in four hospitals in Sudan
Alsmwal Alnour Alnzaer1, Ali Yasen Yasen Mohamedahmed1,&, Yousif Abdalla Adam1, Elmoiz Eltyiep1, Suliman Hussen Suliman2
1General Surgery, Sudan Medical Specialization Board, Khartoum, Sudan, 2Department of General Surgery, University of Khartoum, Khartoum, Sudan
&Corresponding author
Ali Yasen Yasen Mohamedahmed, General Surgery, Sudan Medical Specialization Board, Khartoum, Sudan
Introduction: diverticular disease (DD) was thought to be more prevalent in the western countries, especially the white populations, but the recent increase in incidence among African and Asian population, was reported. Up to our knowledge, there is no previous study of DD in Sudan.
Methods: this is a descriptive cross-sectional study conducted at the department of endoscopy in four Sudanese hospitals in the period from October 2017 to February 2019. We included all patients who underwent colonoscopy during the study period. The main objective is to study the presentation and the anatomical pattern of diverticular disease among the Sudanese population.
Results: prevalence of DD in the included population was 7.5% (104/1393). The mean age was 66.4 ± 12.5 years with the percentage of males in our study is 77.1% and females were 22.9%. Presenting complains were: abdominal pain in all patients, constipation in 78.8% and rectal bleeding in 57.7%. Regarding anatomical distribution: 63.5% have left colonic DD, 19.2% in the right colon and 17.3% involving the entire colon. There was a significant correlation between the left side DD and following clinical presentations: mucus per-rectum (p = 0.015) and weight loss (p = 0.048). Other endoscopic findings of significance were internal pile in 21.2% and colo-rectal polyp in 15.4%.
Conclusion: the prevalence of DD in the included population, is 7.5% which is consistent with recent literature from the Middle East, Africa and Asia but still less than the prevalence in the western countries and left side colon is predominantly affected.
Diverticular disease (DD) is a sac-like protrusion of mucosa through the muscular colonic wall. The protrusion occurs in weak areas of the bowel wall through which blood vessels (vasa recta) penetrate. Colonic diverticula are usually pseudo-diverticula, as they contain only mucosa and sub-mucosa covered by serosa [1-3]. The incidence of DD demonstrates a clear age dependency, although a slight increase in younger patients was observed during the last decade [4, 5]. Lack of dietary fibre, smoking, high body mass index (BMI), alcohol consumption and nonsteroidal anti-inflammatory drugs (NSAIDS) are firmly anchored to DD in the literature [6-10]. Moreover, the following rare syndromes demonstrate a strong predisposition for colonic diverticula formation; Marfan syndrome, Ehlers-Danlos syndrome, Williams-Beuren syndrome, Coffin-Lowry syndrome and polycystic kidney disease [5, 11, 12]. For many years it has been thought that DD exclusively affects westernized countries due to a lack of fibre in the diet, which leads to increase the pressure on the colonic wall [13]. However, recent data has revealed an increase in the prevalence of colonic diverticulosis throughout the world [14]. A low prevalence of diverticulosis was reported in patients who underwent colonoscopy in African countries; ranging from 2% to 13.5% [14-16]. However, a higher incidence was reported in Asian countries, which was up to 28.5% with predominantly on the right side [17, 18]. Much higher prevalence was reported in western countries (57.7% in the USA, 47% in the UK, 49% in Germany, 50% in Finland and 19.9% in Italy) and affecting the left colon in the vast majority of cases [19-23]. In light of this vast ethnicity variation and lack of reports from Sudan regarding pattern and anatomical distribution of DD, we conducted this study to evaluate the pattern of DD in the Sudanese population.
This is a descriptive observational study that was conducted in the endoscopy department in four major Sudanese hospitals: Soba University Hospital, Ibn Sina Specialized Hospital, Omdurman Military Hospital and Alribat Teaching Hospital, in the period from February 2017 to February 2019. All the hospitals mentioned above have an endoscopy unit with consultant physicians and surgeons performing the endoscopy lists and most of the people who required colonoscopy in Khartoum State are referred to one of these hospitals. We include all patients who underwent colonoscopy irrespective if DD is suspected or not.
Inclusion and exclusion criteria: we include all patients attending the endoscopy units in the above-mentioned hospitals during the study period and had a colonoscopy to investigate gastrointestinal symptoms such as: changes in bowel habits, rectal bleeding, anaemia unexplained weight loss. Exclusion criteria were: patients with inadequate bowel preparations, an incomplete examination of the colon and patients who are unwilling to participate in the study. Patients that were confirmed to have DD on colonoscopy were studies to understand the possible risk factors and anatomical distribution. Rectal bleeding was considered major when it required admission to the hospital, such as association with systolic blood pressure less than 90, bleeding that required blood transfusion or persistence of bleeding for more than three days. Moderate rectal bleeding is three episodes or more of rectal bleeding (fresh or dark), or melaena in a haemodynamically stable patient. Two or fewer episodes of rectal bleeding without the previously mentioned criteria were considered as mild rectal bleeding. Data were analysed with statistical package for the social sciences (SPSS) version 23. Qualitative data were analysed using correlation test and simple linear regression and the P-value was considered significant if less than 0.05. Written informed consent obtained from each participant and ethical clearance was obtained from the ethical committee of Sudan Medical Specialization Board, as well as hospital administration approval.
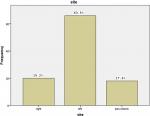
The total number of patients who underwent colonoscopy during the period of study were 1393 patients and 104 of them were confirmed to have DD with a prevalence of 7.5%. Furthermore, patients who confirmed to have DD were identified and studies for baseline characteristics, clinical presentation and risk factors. The mean age was 66.4±12.5 and 70.2% of patients were male. Baseline characteristics and risk factors for diverticulosis in the study population are shown in Table 1. Moreover, 61 out of all patients have medical comorbidities; hypertension was noted in 49.2%, diabetes was noted in 27.9% and 11.5% has ischaemic heart disease. Abdominal pain was the presenting symptom in all patients confirmed to have DD with left iliac fossa pain reported in 58.6%, right iliac fossa reported in 21.1% and generalized abdominal pain reported in 20.2%. In addition, rectal bleeding was the presenting symptom in 57.6% and the degree of bleeding were described as major in 9.6% of patients, moderate in 26% of patients and minor in 22.1% of patients. Table 2 shows clinical presenting symptoms. Regarding the anatomical distribution of colonic diverticulosis, more than half of the cases (63.5%) had left colonic diverticulae, 19.2% of patients have colonic diverticulae in the right colon and in 17.3% the disease involved the entire colon (Figure 1). Furthermore, the left side diverticulae showed a statistically significant higher risk for mucus per-rectum (P-value=0.015) and weight loss (P-value=0.048). However, there was no statistically significant risk between the site of diverticulae and the following outcomes: rectal bleeding (P-value=0.496), bowel habits (P-value=0.87), abdominal bloating (P-value=0.135), anaemic symptoms (P-value=0.519), anorexia (P-value=0.154) and constipation (P-value=0.207) (Table 3). Other endoscopic findings of significance were internal pile in 21.2% and colo-rectal polyp in 15.4%, other outcomes like colitis and masses occur less frequently (Table 4).
Diverticular disease (DD) was thought to be more prevalent in the western world especially the white populations, but the recent increase in incidence among the immigrants from Africa who reside in the west for more than ten years may indicate that the westernization of the lifestyle could be the cause for this change in DD epidemiology [1, 23, 24]. In Africa, the Middle East and Asia the prevalence is less [14-18, 25-27]. In this study the prevalence of DD was 7.5% (104/1393) among all patients who underwent a colonoscopy to investigate gastro-intestinal symptoms which is comparable to a prevalence of 7.4% that reported previously in Saudi Arabia [27]. However, a higher prevalence of 13.5% and 12.1% were reported in studies from South Africa and North Korea, respectively [26, 28]. The prevalence in western countries is much higher 47% in the UK and up to 49% in Germany [21, 22]. The mean age was 67 ± 12.7 in this study which is similar to the reports from Africa and USA [16, 19, 27] but far different from Asian reports from Saudi Arabia with a mean age of 60.82 ± 0.833 and North Korea with a mean age of 50.9 ± 12.3 [27, 28]. The youngest patient in our study was 17 years of age. The youngest patient with colonic diverticulosis was described by Ignacio RC Jr who reported a 9 years old patient with William syndrome presented with rectal bleeding secondary to sigmoid diverticulitis [29].
The percentage of males in our study is 77.1% and females were 22.9% which is consistent with previous studies from Africa, the USA and Europe [16, 19, 27]. Risk factors for colonic diverticulosis include: low fibre diet, increased age, smoking, obesity, lack of exercise and certain medications (NSAIDs, anticoagulants and corticosteroid ) [1, 15, 19, 25, 27, 28]. Sixty one patients were found to have one or more medical comorbidity in this study. Hypertension was found to be associated with increased risk of bleeding from DD, which is predominantly due to vascular endothelial injury and atheroma formation that leads to arteriosclerosis and increased pressure within exposed blood vessels which elevates the risk for bleeding [27]. A fifth of the included population (20.1%) showed a degree of obesity. However, there was no significant relation between obesity and rectal bleeding in this study (P-value=0.09). Several reports have shown that obesity increased the risk of DD complications, including rectal bleeding [30, 31]. A study from Sweden reported that obese patients with diverticular disease have a higher risk of hospitalization [32]. This may be due to the suggested link between obesity and inflammation along with intestinal flora differences in obese population [33]. Patients with DD can present with non-specific abdominal complaints, e.g. left-sided lower abdominal pain.
Patients with DD do not usually manifest signs of inflammation, such as pyrexia or neutrophilia, which could indicate diverticulitis. Pain is generally exacerbated by eating and diminished with defecation or flatus, suggesting colonic wall tension due to raised intraluminal pressure. Complicated DD presents according to the nature of the complication, which is predominantly abscess formation, perforation, Fistulation, bleeding, stricture or obstruction. Abscess formation is the most common presentation of acute complicated diverticulitis which occurs in approximately 15% of patients [1, 2]. A significant localized abscess may progress into a free perforation in 1-2% of patients with DD, which is associated with high morbidity and mortality [1, 2]. All patients in this study complained of abdominal pain at some point of the disease course. While the risk of bleeding from colonic diverticulosis is known to be around 15%; in this study, more than half the patients have rectal bleeding and 33.7% of patients were confirmed to have symptomatic anaemia. The mechanism of DD bleeding is thought to be due to rupture of the vasa recta at the neck of the diverticulum [34]. However, diverticular bleeding stops spontaneously in 90% of patients, there is a high risk for recurrence most commonly in patients with bilateral diverticulosis, on NSAIDs or anticoagulants [35-37].
In this study, we found that there is no statistically significant association between the degree of bleeding and smoking (p=0.526), NSAIDs (p=0.132) or different medical comorbidities (p=0.248). There is a clear overlap of symptoms between DD and different colonic pathologies, e.g. inflammatory bowel disease (IBS) and malignant tumours, the reason why a colonoscopy is becoming the gold standard investigation in patients with lower gastro-intestinal symptoms [1, 2, 23]. The anatomical site of the diverticula in this study was left site predominance with a percentage of 61.4% and this is consistent with studies from Europe and the USA [38]. However, reports from the Middle East and Africa revealed that the right side involved more frequently [1, 23, 27, 28, 38-41]. Association between colonic adenoma and DD was proposed by several authors as both shared common epidemiological trends and risk factors such as increased age and low fibre diet [42, 43]. An increased risk of 1.7-fold and 2.3-fold for colonic polyps in patients with DD were revealed among Japanese and African-American population respectively [44, 45]. In this study, 15.4% of patients with the diverticular disease were found to have colonic polyps.
The prevalence of DD was 7.5% in patients who underwent a colonoscopy to investigate lower gastro-intestinal symptoms in this study, which is consistent with recent literature from the Middle East, Africa and Asia but still less than the prevalence in the western countries. The most common presentation is abdominal pain and rectal bleeding. The diverticular disease in this study is mainly left-sided which is not similar to reports from other countries in Asia and Africa where right side diverticular disease predominate. More studies are needed to investigate the outcome of treatment in the Sudanese population.
What is known about this topic
- No published research about presentation and anatomical distribution of DD in Sudan;
- Prevalence of DD is rising in Africa.
What this study adds
- The prevalence of the diverticular disease in the included population is 7.5%;
- Most common presentation in the study population is abdominal pain and rectal bleeding;
- The diverticular disease in the included population is mainly left-sided.
The authors declare no competing interests.
AAA, AYM, SHS conceived the idea of the study; AAA, AYM, YAA, EE contributed equally to data collection and data analysis; AAA, AYM, YAA,EE, AAH contributed to manuscript writing and review of the manuscript. All the authors have read and agreed to the final manuscript.
Table 1: shows demographic characteristics of included population and risk factors
Table 2: shows clinical presentation of included population
Table 3: relationship between side of the diverticulosis and clinical presentation
Table 4: other significant findings during the colonoscopy
Figure 1: anatomical distribution of colonic diverticulosis
- Neil S, Jeffrey BR. Diverticular disease of the colon. Lancet. 2004 Feb 21;363(9409):631-9. PubMed | Google Scholar
- Parks TG. Natural history of diverticular disease of the colon. Clin Gastroenterology. 1975;4(1):p 53-69. PubMed | Google Scholar
- Murphy T, Hunt RH, Fried M, Krabshuis JH. World gastroenterology organisation practice guidelines: diverticular Disease. World Gastroenterology Organisation. 2013;p5-9.
- Bohm SK. Risk factors for diverticulosis, diverticulitis, diverticular perforation and bleeding: a plea for more subtle history taking. Viszeralmedizin. 2015 Apr;31(2):84-94. PubMed | Google Scholar
- Weizman AV, Nguyen GC. Diverticular disease: epidemiology and management. Can J Gastroenterol. 2011;25(7):385-389. PubMed | Google Scholar
- Marc RM, David AM. Epidemiology and pathophysiology of diverticular disease. Clin Colon Rectal Surg. 2009 Aug;22(3):141-146. PubMed | Google Scholar
- Strate LL. Lifestyle factors and the course of diverticular disease. Dig Dis. 2012;30(1):35-45. PubMed | Google Scholar
- Hjern F, Wolk A, Hakansson N. Smoking and the risk of diverticular disease in women. Br J Surg. 2011;98(7):997-1002. PubMed | Google Scholar
- Corder A. Steroids, non-steroidal anti-inflammatory drugs and serious septic complications of diverticular disease. Br Med J. 1987;295(6608):1238. PubMed | Google Scholar
- Langman MJS, Morgan L, Worrall A. Use of anti-inflammatory drugs by patients admitted with small or large bowel perforations and haemorrhage. Br Med J (Clin Res Ed). 1985;290(6465):47-349. PubMed | Google Scholar
- Petruzziello L, Iacopini F, Buljic, Shah M, Costamagna G. Review article: uncomplicated diverticular disease of the colon. Aliment Pharmacol Ther. 2006;23(10):1379-1391. PubMed | Google Scholar
- Jun S, Stollman N. Epidemiology of diverticular disease. Best Pract Res Clin Gastroenterol. 2002;16(4):529-542. PubMed | Google Scholar
- Floch M, Bina I. The natural history of diverticulitis - fact and theory. J Clin Gastroenterol. 2004;38(5 Suppl. 1):S2-S7. PubMed | Google Scholar
- Alatise O, Arigbabu A, Agbakwuru E, Lawal O, Ndububa D, Ojo O. Spectrum of colonoscopy findings in Ile-Ife Nigeria. Niger Postgrad Med J. 2012;19(4):219-224. PubMed | Google Scholar
- Elbatea H, Enaba M, Elkassas G, El-Kalla F, Elfert A. Indications and outcome of colonoscopy in the middle of Nile delta of Egypt. Dig Dis Sci. 2011;56(7):2120-2123. PubMed | Google Scholar
- Vally M, Koto MZ, Govender M. An investigation of diverticular disease among black patients undergoing colonoscopy at Dr George Mukhari Academic Hospital, Pretoria, South Africa. South Africa Medical Journal. 2017;107(2):137-139. PubMed | Google Scholar
- Lohsiriwat V, Suthikeeree W. Pattern and distribution of colonic diverticulosis: analysis of 2877 barium enemas in Thailand. World J Gastroenterol. 2013;19(46):8709-8713. PubMed | Google Scholar
- Nagata N, Niikura R, Aoki T, Shimbo T, Itoh T, Goda Y et al. Increase in colonic diverticulosis and diverticular hemorrhage in an aging society: lessons from a 9-year colonoscopic study of 28,192 patients in Japan. Int J Colorectal Dis. 2014;29(3):379-385. PubMed | Google Scholar
- Smoot D, Collins J, Dunlap S, Ali-Ibrahim A, Nouraie M, Lee EL et al. Outcome of colonoscopy in elderly African-American patients. Dig Dis Sci. 2009;54(11):2484-2487. PubMed | Google Scholar
- Mehrzad R, Mishra S, Faller G, Memon B, Fiore J. Right-sided diverticulosis and disparities from left-sided diverticulosis in the Vietnamese population living in Boston, Mass, USA: a retrospective cohort study. Med Princ Pract. 2015;24(4):355-361. PubMed | Google Scholar
- Delvaux M. Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther. 2003;18(Suppl. 3):71-74. PubMed | Google Scholar
- Weismüller T, Bleich F, Negm A, Schneider A, Lankisch T, Manns M et al. Screening colonoscopy in liver transplant candidates: risks and findings. Clin Transplant. 2013;27(2):E161-E168. PubMed | Google Scholar
- Tursi A, Brandimarte G, Di Mario F, Andreoli A, Annunziata ML, Astegiano M et al. Development and validation of an endoscopic classification of diverticular disease of the colon: the DICA classification. Dig Dis. 2015;33(1):68-76. PubMed | Google Scholar
- Fatayer W, A-Khalaf M, Shalan K, Toukan A, Daker M, Arnaout M. Diverticular disease of the colon in Jordan. Dis Colon Rectum. 1983;26(4):247-249. PubMed | Google Scholar
- Mudawi HMY, Mohammed Ali SEA, Dabora AA, EL Tahir MA, Suliman SH, Salim OE et al. American society for gasterointestinal endoscopy guidelines for appropriate use of colonscopy: are they suitable for African patients. Trop Doct. 2012 Jul;42(3):165-7. PubMed | Google Scholar
- Aboagye E, Agyemang O, Sidney K. Socioeconomic factors and health outcome metrics in Africa: cross-national comparisons from 1995-2011. Popul Health Manag. 2014;17(5):318-319. PubMed | Google Scholar
- Azzamc N, Aljebreen AM, Alharbi O, Almadi MA. Prevalence and clinical features of colonic diverticulosis in a Middle Eastern population. World J Gastrointest Endosc. 2013 Aug 16;5(8):391-397. PubMed | Google Scholar
- Song JH, Kim YS, Lee JH, Ok KS, Ryu SH, Lee JH et al. Clinical characteristics of colonic diverticulosis in Korea: a prospective study. Korean J Intern Med. 2010;25(2):140-146. PubMed | Google Scholar
- Ignacio RC Jr, Klapheke WP, Stephen T, Bond S. Diverticulitis in a child with Williams syndrome: a case report and review of the literature. J Pediatr Surg. 2012 Sep;47(9):E33-5. PubMed | Google Scholar
- Zaidi E, Daly B. CT and clinical features of acute diverticulitis in an urban US population: rising frequency in young, obese adults. AJR Am J Roentgenol. 2006;187(3):689-94. PubMed | Google Scholar
- Alatise OI, Arigbabu AO, Lawal OO, Adetiloye VA, Agbakwuru EA, Ndububa DA. Presentation, distribution pattern and management of diverticular disease in a Nigerian tertiary hospital. Niger J Clin Pract. 2013 Apr-Jun;16(2):226-31. PubMed | Google Scholar
- Rosemar A, Angeras U, Rosengren A. Body mass index and diverticular disease: A 28-year follow-up study in men. Dis Colon Rectum. 2008;51(4):450-5. PubMed | Google Scholar
- Manwaring M, Champagne B. Diverticular disease: genetic, geographic and environmental aspects. Semin Colon Rectal Surg. 2011;22(3):148-53. PubMed | Google Scholar
- Meyers MA, Alonso DR, Gray GF, Baer JW. Pathogenesis of bleeding colonic diverticulosis. Gastroenterology. 1976;71(4):577-83. PubMed | Google Scholar
- McGuire HH Jr. Bleeding colonic diverticula: a reappraisal of natural history and management. Ann Surg. 1994;220(5):653-6. PubMed | Google Scholar
- Lewis M. Bleeding colonic diverticula. J Clin Gastroenterol. 2008;42(10):1156-8. PubMed | Google Scholar
- Taki M, Oshima T, Tozawa K, Taniguchi Y, Tomita T, Ohda Y et al. Analysis of risk factors for colonic diverticular bleeding and recurrence. Medicine (Baltimore). 2017 Sep;96(38):e8090. PubMed | Google Scholar
- Rajendra S, Ho JJ. Colonic diverticular disease in a multiracial Asian patient population has an ethnic predilection. Eur J Gastroenterol Hepatol. 2005;17(8):871-5. PubMed | Google Scholar
- Mokoena T, Madiba TE. Haemorrhagia: the main presenting feature of diverticular disease in blacks. S Afr Med J. 1994;84(2):83-5. PubMed | Google Scholar
- Kiguli-Malwadde E, Kasozi H. Diverticular disease of the colon in Kampala, Uganda. Afr Health Sci. 2002;2(1):29-32. PubMed | Google Scholar
- Baako BN. Diverticular disease of the colon in Accra, Ghana. Br J Surg. 2001;88(12):1595. PubMed | Google Scholar
- Morini S, Hassan C, Zullo A, De Francesco V, Festa V, Barberani F et al. Diverticular disease as a risk factor for sigmoid colon adenomas. Dig Liver Dis. 2002;34(9):635-639. PubMed | Google Scholar
- Aldoori WH, Giovannucci EL, Rockett HR, Sampson L, Rimm EB, Willett WC. A prospective study of dietary fiber types and symptomatic diverticular disease in men. J Nutr. 1998;128(4):714-719. PubMed | Google Scholar
- Hirata T, Kawakami Y, Kinjo N, Arakaki S, Arakaki T, Hokama A et al. Association between colonic polyps and diverticular disease. World J Gastroenterol. 2008 Apr 21;14(15):2411-2413. PubMed | Google Scholar
- Ashktorab H, Panchal H, Shokrani B, Paydar M, Sanderson A, Lee EL et al. Association between diverticular disease and pre-neoplastic colorectal lesions in an urban African-American population. Digestion. 2015;92(2):60-5. PubMed | Google Scholar