A coronary artery aneurysm revealing a Behçet´s disease: a case report
Sameh Ben Farhat, Mehdi Slim
Corresponding author: Sameh Ben Farhat, Department of Cardiology, Sahloul University Hospital, Sousse, Tunisia 
Received: 17 Mar 2020 - Accepted: 22 Apr 2020 - Published: 04 May 2020
Domain: Cardiology
Keywords: Behçet´s disease, coronary aneurysm, acute coronary syndrome
©Sameh Ben Farhat et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Sameh Ben Farhat et al. A coronary artery aneurysm revealing a Behçet´s disease: a case report. Pan African Medical Journal. 2020;36:3. [doi: 10.11604/pamj.2020.36.3.22373]
Available online at: https://www.panafrican-med-journal.com//content/article/36/3/full
A coronary artery aneurysm revealing a Behçet´s disease: a case report
Sameh Ben Farhat1,&, Mehdi Slim1
1Department of Cardiology, Sahloul University Hospital, Sousse, Tunisia
&Corresponding author
Sameh Ben Farhat, Department of Cardiology, Sahloul University Hospital, Sousse, Tunisia
Behçet´s disease (BD) is a multisystemic chronic vasculitis characterized by its clinical polymorphism. It concerns mainly young men and generally appears between the third and the fourth decades. Cardiac involvement in Behçet´s disease is rare but represents a major prognostic factor. We report the case of a young man admitted in our department for the management of an acute coronary syndrome revealing a Behçet´s disease. Coronary angiography had shown a giant thrombosed aneurysm of the left coronary artery. Surgical treatment was successfully performed and the patient had a left anterior descending coronary artery bypass using the left internal mammary artery graft.
First described in 1937, Behçet´s disease (BD) is defined as a chronic multisystemic inflammatory condition affecting small, medium and large-caliber vessels [1, 2]. Its prevalence varies widely from one region to another and is particularly high in the Middle and Far East [3]. Genetic, environmental or autoimmune factors have been implicated in its etiopathogenesis, however, the exact etiology remains unclear [2]. The disease usually appears during the 3rd or the 4th decade with a peak frequency around the age of 30 [1]. Both men and women could be affected, but there is a slight male predominance [4]. Cardiac involvement in BD is uncommon, however, it is clearly associated with a poor prognosis [2]. We report the case of a young man admitted in our department for acute coronary syndrome secondary to a thrombosed aneurysm of the left anterior descending coronary artery and revealing an angiobehçet.
A 32-year-old man, with no cardiovascular risk factors, was admitted in our department for typical chest pain that had been exaggerated in the last week. In his past medical history, he had a left hip synovitis treated with corticosteroids and a recurrent oral aphthosis. Cardiovascular examination was unremarkable; however, bilateral ulcerated scrotal lesions were noted. Electrocardiography (EKG) showed a non-persistent ST segment elevation in the lateral leads. Laboratory data revealed elevated cardiac troponin and C-reactive protein at a concentration of 4.71 µg/L and 100 mg/L respectively while other blood tests were within the standard limits.
Transthoracic echocardiography (TTE) was normal. He received antithrombotic therapy followed by a coronary angiography that showed multiple aneurysms of the main diagonal branch and the left circumflex coronary artery. The largest one measured 8 mm and was located in the bifurcation of the left anterior descending coronary artery (LAD) with the first diagonal branch. BD was strongly suspected and the patient was transferred to medicine department where the diagnosis was confirmed. He received immunosuppressive therapy that induced total remission of his disease and complete resolution of angina.
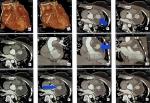
A year later, he was readmitted for unstable angina. His physical examination was strictly normal. EKG showed regular sinus rhythm with ST segment depression in inferior and apicolateral leads (Figure 1). Blood tets revealed biological inflammatory syndrome but no elevation in the level of the myocardial markers of necrosis. Transesophageal echocardiography (TEE) revealed preserved biventricular function. Though, there was a huge aneurysmal mass measuring approximately 58*47 mm, arising from the left coronary artery and distorting the lateral wall of the left ventricle (LV) and the pulmonary artery (PA) without creating an authentic right outflow tract obstruction (Figure 2). We performed coronary angiography that showed a severe stenotic lesion of the proximal segment of the LAD localized opposite to a huge aneurysm of about 3 cm in size inducing a coronary steal phenomenon with a delayed opacification of the distality of the vessel (Figure 3). On computed tomography (CT) angiography, there was a saccular thrombosed aneurysm of the proximal segment of the LAD measuring 3cm with a neck portion of 4.3mm (Figure 4). Two other small aneurysms of the second diagonal branch of 3 and 4 mm of diameter respectively were also noted.
Surgery was performed after inflammation control. Peroperative exploration identified the aneurysmal sac filled with a big thrombus and contacting the lateral wall of the LV and the PA (Figure 5). Surgeons proceeded to open and resect the aneurysm then sutured the neck portion. Afterward they performed a bypass of the LAD using the left internal mammary artery graft. The postoperative period went without incident and the patient was successfully discharged.
Cardiac involvement is rare but severe during BD. Its prevalence varies from 0.36 to 19.5 per 100,000 inhabitants depending on the clinical series [1, 5]. All three layers of the cardiac wall can be affected. Thus, cardiac manifestations may include, pericarditis (20 to 40%), myocarditis (20%), endocarditis, endomyocardial fibrosis or myocardial infarction [6]. The coronary arteries are rarely involved (prevalence of 0.5%) by stenotic lesions, arteritis or especially aneurysms formation [4].
Physiologically, vascular involvement could be explained by the deposition of immune complexes in the vascular wall leading to a subsequent complement-activated leukocyte infiltration [4]. The inflammatory infiltrate made of plasma cells and lymphocytes affects preferably the media, the adventitia and the vasa-vasorum causing an abnormal weakening and thinning of the blood vessels wall with the formation of aneurysms and pseudoaneurysms which constitutes an authentic arterial aphtosis [1].
Behçet disorder is rarely inaugurated by coronary artery disease. In fact, most cases reported in the literature were already diagnosed and treated for this condition [2]. Typical clinical picture is represented by acute coronary syndrome and the first case was reported by Schiff et al in 1982 [7]. Several mechanisms have been described in the literature: coronary occlusions secondary to vasculitis, the formation of thrombus in situ, compression of the vessels by an aneurysm or dilated valsalva sinus or less frequently an impairment of the microvascular function [2, 8]. The modalities for the management of coronary artery disease during BD are based on the decision of a multidisciplinary team including the internist, the cardiologist and the cardiovascular surgeon. In general, in addition to standard anti-ischematic therapy, the combination of corticosteroids with immunosuppressive drugs is highly recommended [9].
Complete remission can be achieved by medical treatment alone and some aneurysms may even completely regress. Nevertheless, surgical or endovascular approaches are deemed necessary in most circumstances. Surgery is recommended for giant aneurysms (size greater than 2 cm), with fast progression and high risk of rupture [3]. In other cases, surgical or interventional management can be discussed [4, 10, 11]. These two techniques may, however, carry more risk of disease progression which is inherent to their pathergy-like effects [12]. Several measures can reduce this risk, such as optimal control of inflammation in the preoperative period, careful examination of arterial or venous grafts before their implantation, and avoiding excessive manipulation of the aorta [2, 12].
Coronary involvement during BD is rare but serious. Angiographically, the most commonly found coronary lesions are aneurysms for which treatment could be surgical or endovascular. Due to the unpredictable evolution of this condition and insufficient data concerning the medium and long-term results of both surgical and interventional techniques, long-term follow-up is required.
The authors declare no competing interests.
Sameh Ben Farhat: drafting the article; Mehdi Slim: final approval. Both authors read and agreed to the final version of this manuscript.
Figure 1: electrocardiogram showing ST segment depression in inferior and apico-lateral leads
Figure 2: transesophageal echocardiography, short axis view showing an aneurysmal mass contacting the pulmonary artery
Figure 3: coronary angiography revealing a thrombosed aneurysm of the left coronary artery
Figure 4: CT angiography identifying a saccular thrombosed aneurysm of the proximal segment of the LAD
Figure 5: peroperative view of the thrombus filling the aneurysmal sac
- Hatemi G, Seyahi E, Fresko I, Talarico R, Hamuryudan V. One year in review 2019: Behçet´s syndrome. Clin Exp Rheumatol. Nov-Dec 2019;37 Suppl 121(6):3-17 Epub 2019 Dec 9. PubMed | Google Scholar
- Farouk H, Zayed HS, El-Chilali K. Cardiac findings in patients with Behçet´s disease: Facts and controversies. Anatol J Cardiol. 2016 Jul;16(7):529-33. PubMed | Google Scholar
- Román Rego A, García Acuña JM, Àlvarez Rodríguez L, Rigueiro Veloso P, López Otero D, González Juanatey JR. Cardiac Involvement in a Patient With Behçet´s disease. Diagnostic and Therapeutic Approach. Rev Espanola Cardiol Engl Ed. 2018 Dec;71(12):1075-1077 Epub 2017 Dec 6. PubMed | Google Scholar
- Liu H-F, Wang M, Xu Y-S, Lu X-R, Lei J-Q. Left Circumflex pseudoaneurysm and left anterior descending Aneurysm in Coronary Artery Due to Behcet´s Disease. Chin Med J (Engl). 2018 Nov 5;131(21):2626-2627. PubMed | Google Scholar
- Chen J-Y, Tsai Y-S, Li Y-H. Multiple arterial aneurysms in a patient with Behçet´s disease. Eur Heart J - Cardiovasc Imaging. 2016 May;17(5):587 Epub 2016 Feb 6. PubMed | Google Scholar
- Bennaser M, Jaziri F, Benjazia A, Hentati O, Euch ME, Mahfoudhi M et al. L´atteinte cardiaque au cours de la maladie de Behçet. Rev Médecine Interne. 2017;38:A187. Google Scholar
- Schiff S, Moffatt R, Mandel WJ, Rubin SA. Acute myocardial infarction and recurrent ventricular arrhythmias in Behcet´s syndrome. Am Heart J. 1982 Mar;103(3):438-40. PubMed | Google Scholar
- Gürkan U, Kaya A, Tatlisu MA, Avsar S. A case report of coronary artery aneurysm in a patient with Behçet´s disease. Turk Kardiyol Dernegi Arsivi Turk Kardiyol Derneginin Yayin Organidir. 2014 Oct;42(7):651-4. PubMed | Google Scholar
- Yuan S-M. Cardiovascular operations in Behçet´s disease. Int J Cardiol. 2014 Mar 1;172(1):e28-9. PubMed | Google Scholar
- Calafiore AM, Helali SA, Iaco´ AL, Sheickh AA, Kheirallah H, Mauro MD. A Giant Pseudoaneurysm of the left anterior descending coronary artery related to Behçet´s disease. Ann Thorac Surg. 2015 Mar;99(3):e59-61. PubMed | Google Scholar
- Kwon CM, Lee SH, Kim JH, Lee KH, Kim HD, Hong YH et al. A case of Behçet´s disease with pericarditis, thrombotic thrombocytopenic purpura, deep vein thrombosis and coronary artery pseudo aneurysm. Korean J Intern Med. 2006 Mar;21(1):50-6. PubMed | Google Scholar
- Husain A, Al-Allaf A, Alamri M, AlKalbani A. Progressive coronary aneurysms in Behçet´s disease, a journey through surgical and percutaneous treatment: A case report. J Cardiol Cases. 2016 Apr 14;14(1):32-34. PubMed | Google Scholar