Spermatic vein thrombosis with lupus anticoagulant, a cause of acute inguinal pain: a case report
Mohammed Aynaou, Tarik Mhanna, Amine Elhoumaidi, Paapa Dua Boateng, Ali Barki
Corresponding author: Mohammed Aynaou, Department of Urology, Mohamed VI university hospital center, Mohamed First Oujda, Morroco 
Received: 25 Sep 2019 - Accepted: 06 Jun 2020 - Published: 25 Jun 2020
Domain: Urology
Keywords: Spermatic vein, thrombosis, lupus anticoagulant
©Mohammed Aynaou et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Mohammed Aynaou et al. Spermatic vein thrombosis with lupus anticoagulant, a cause of acute inguinal pain: a case report. Pan African Medical Journal. 2020;36:125. [doi: 10.11604/pamj.2020.36.125.20448]
Available online at: https://www.panafrican-med-journal.com//content/article/36/125/full
Case report 
Spermatic vein thrombosis with lupus anticoagulant, a cause of acute inguinal pain: a case report
Spermatic vein thrombosis with lupus anticoagulant, a cause of acute inguinal pain: a case report
Mohammed Aynaou1,&, Tarik Mhanna1, Amine Elhoumaidi1, Paapa Dua Boateng1, Ali Barki1
&Corresponding author
Patients with lupus anticoagulants are at high risk of systemic arterial and venous thrombosis and arterial stroke. We present an unusual case of a young man presenting inguinal pain. Doppler ultrasound revealed spermatic vein thrombosis on the left side. Hematologic workup revealed positive lupus anticoagulant. The patient was treated with therapeutic heparin.
Spermatic vein thrombosis is a rare event which can be difficult to diagnose. Multiple predisposing factors have been associated with Spontaneous Spermatic vein thrombosis, like malignant tumors, coagulopathies and varicocele [1]. We present a case of spermatic vein thrombosis in the left spermatic vein.
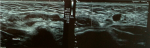
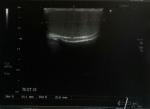
A 27-year-old male, with no previous health problems, was admitted with a 1-week history of painful in the left inguinal region, without fever or any associated signs. He denied any etiologic factors like trauma, surgeries, severe exercise or thrombogenic factors. Inguinal region, scrotum and prostate were normal to palpation. Initial laboratory test, were normal. Doppler ultrasonography of left inguinal region demonstrated an expanded vein which contained thrombus (Figure 1) with no blood flow at Doppler (Figure 2). Scrotal Doppler ultrasound (Figure 3) and Total abdomen contrast-enhanced CT examination excluded other diseases (Figure 4). Complete biology workup was negative, except lupus Anticoagulant was positive. A medical treatment of anticoagulant at a curative dose was started. After 15 days, the patient´s inguinal pain was completely disappeared. Three months later, inguinal ultrasound revealed no residual evidence of spermatic vein thrombosis.
Spermatic vein thrombosis is a rare pathology, it can clinically simulate an incarcerated hernia [2]. In addition, there is another differential diagnosis such as spermatic cord torsion, benign and malignant tumors of spermatic cord [3-5]. Several etiologic factors are associated with spermatic vein thrombosis, likes trauma to the vascular endothelium, obstruction to venous drainage, hypercoagulable states, vigorous sexual activity or sport activity, infection, tumors of the genitor urinary tract and inguinal hernia surgery etc. [6]. Doppler ultrasound offers a non-invasive and accurate means of establishing and confirming the diagnosis. Lupus anticoagulants are associated with an increased incidence of venous and arterial thrombotic events [7-9]. In the literature we report cases of venous thrombosis of pulmonary [9], retinal [10], renal [11] and cerebral [12]. Several mechanisms of thrombosis induced by lupus anticoagulant includes antiphospholipid activity [13], inhibition of prostacyclin formation [14], prekallikrein inhibition [15] and direct injury of the vessel wall by an antibody-antigen complex [8]. The management of thrombosis of spermatic vein is controversial. For Thrombosis venous localized out of external inguinal ring we can propose conservative management including watchful observation. Whereas for deep seated spermatic vein thrombus inside the external inguinal ring, surgical approach May prevent pulmonary embolism. Anticoagulant therapy can be used clinically.
Spermatic vein thrombosis is particularly rare disease. Ultrasound should be the first line examination to avoid exploratory surgery.
The authors declare no competing interests.
Mohammed Aynaou, Tarik Mhanna, Amine Elhoumaidi and Paapa Dua Boateng contributed to the design and implementation of the research and to the writing of the manuscript. Ali Barki supervised the manuscript. All of them have read and agreed to the final manuscript.
Figure 1: ultrasonography demonstrated tubular structure hypoechoic non compressed consistent with thrombus
Figure 2: color Doppler signal was not presented inside the hypoechoic structure
Figure 3: left testicular without abnormality
Figure 4: absence of renal masses on the abdominal CT scan
- Hashimoto L, Vibeto B. Spontaneous thrombosis of the pampiniform plexus. Scand J Urol Nephrol. 2006;40(3):252-4. PubMed | Google Scholar
- Isenberg JS, Ozuner G, Worth MH, Ferzli G. Effort induced spontaneous thrombosis of the left spermatic vein presenting clinically as a left inguinal hernia. J Urol. 1990 Jul;144(1):138. PubMed | Google Scholar
- kleinclauss F, Della Negra E, Martin M, Bernardini S, Bittard H. Spontaneous thrombosis of left varicocele. Prog Urol. 2001 ;11(1):95-6. PubMed | Google Scholar
- Campagnola S, Flessati P, Fasoli L, Sulpasso M, Pea M. A rare case of acute scrotum. Thrombophlebitis from ectasia of the left pampiniforme plexus. Minerva Uroll Nephrol. 1999 Sep;51(3):163-5. PubMed | Google Scholar
- Gleeson MJ, McDermott M, McDonald G, McDermott TE. Spontaneous thrombosis of the left spermatic vein. Bt J Urol. 1992 Nov;70(5):567. PubMed | Google Scholar
- Kayes O, Patrick N, Sengupta A. A peculiar case of bilateral, spontaneous thromboses of the pampiniform plexi. Ann R Coll Surg Engl. 2010 Oct;92(7):W22-3. PubMed | Google Scholar
- Harris EN, Gharavi AE, Hughes GRV. Antiphospholipid anti-bodies. Clin rheum Dis. 1985;11(3):591-609. PubMed | Google Scholar
- LeRoux G, Wautier M-P, Guillevin L, Wautier J-L. IgG binding to endothelial cells in systemic lupus erythematosus. Thromb HAEMOST. 1986 Oct;56(2):144-146. PubMed | Google Scholar
- Mueh JR, Herbst KD, Rapaport IS. Thrombosis in patients with the lupus anticoagulant. Ann Intern Med. 1980 Feb;92(2 Pt 1):156-15. PubMed | Google Scholar
- Silverman M, Lubeck Mj, Briney WG. Central retinal vein occlusion complicating systemic lupus erythematosus. Arthritis Rheum. 1978 Sep-Oct;21(7):839-843. PubMed | Google Scholar
- Asherson RA, Lanham JG, Hull RG, Boey ML, Gharavi AE, Hughes GRV. Renal vein thrombosis in systemic lupus erythematosus. Association with the lupus anticoagulant. Clin Exp Rheumatol. 1984 Jan-Mar;2(1):75-79. PubMed | Google Scholar
- Averback P. Primary cerebral venous thrombosis in young adults: The diverse manifestations of an underrecognized disease. Ann Neurol. 1978 Jan;3(1):81-86. PubMed | Google Scholar
- Thiagarajan P, Shapiro SS, Demarco L. Monoclonal immunoglobulin M-Lambda coagulation inhibitor with phospholipid specificity. Mechanism of a lupus anticoagulant. J Clin invest. 1980 Sep;66(3):397-405. PubMed | Google Scholar
- Carrera LO, Vermylen JG. Lupus anticoagulant and thrombosis-Possible role of inhibition of prostacyclin formation. Thromb Haemost. 1982 Aug;48(1):38-40. PubMed | Google Scholar
- Samnfelippo MJ, Drayna CJ. Prekallikrein inhibition associated with the lupus anticoagulant. Am J Clin Pathol. 1982 Mar;77(3):275-279. PubMed | Google Scholar