Knowledge, risk perception, and condom utilization pattern among female sex workers in Dire Dawa, Eastern Ethiopia 2016: a cross-sectional study
Hailemariam Mekonnen Workie, Teshager Worku Kassie, Tewodros Tesfa Hailegiyorgis
Corresponding author: Hailemariam Mekonnen Workie, Haramaya University, college of health and medical science, school of nursing and Midwifery, Harar, Ethiopia 
Received: 25 Jul 2018 - Accepted: 05 Dec 2018 - Published: 16 Apr 2019
Domain: Community health,Public health,Reproductive Health
Keywords: HIV/AIDS, knowledge, risk perception, condom, utilization, female sex workers, Ethiopia
©Hailemariam Mekonnen Workie et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Hailemariam Mekonnen Workie et al. Knowledge, risk perception, and condom utilization pattern among female sex workers in Dire Dawa, Eastern Ethiopia 2016: a cross-sectional study. Pan African Medical Journal. 2019;32:185. [doi: 10.11604/pamj.2019.32.185.16574]
Available online at: https://www.panafrican-med-journal.com//content/article/32/185/full
Original article 
Knowledge, risk perception, and condom utilization pattern among female sex workers in Dire Dawa, Eastern Ethiopia 2016: a cross-sectional study
Knowledge, risk perception, and condom utilization pattern among female sex workers in Dire Dawa, Eastern Ethiopia 2016: a cross-sectional study
Hailemariam Mekonnen Workie1,&, Teshager Worku Kassie1, Tewodros Tesfa Hailegiyorgis2
1Haramaya University, College of Health and Medical Science, School Of Nursing and Midwifery, Harar, Ethiopia, 2Department of Medical Laboratory Science, College of Medical and Health Sciences, Haramaya University, Harar, Ethiopia
&Corresponding author
Hailemariam Mekonnen Workie, Haramaya University, college of health and medical science, school of nursing and Midwifery, Harar, Ethiopia
Introduction: in 2015, in Dire Dawa administration city, adult HIV prevalence was 3.26 with 9,523 HIV positive population, & 251 annual AIDS deaths. Female sex workers are one of the high-risk groups for contracting HIV. Therefore, this study has assessed the level of HIV/AIDS knowledge, risk perception and condom utilization pattern among female sex workers' in Diredawa city.
Methods: a cross-sectional study was conducted from April 15-June 25, 2016, in Dire Dawa among 156 female sex workers using convenient sampling method. Respondents were interviewed face-to-face using a pretested questionnaire. Training was provided to the data collectors and supervisors. Close supervision was done and double data entry was performed. Then the data were checked for completeness, consistency and entered into Epi Info v3.1 and analyzed using SPSS v20. The descriptive statistical analysis was used to compute frequency, mean, mode and proportion of the findings of this study. The results were presented using tables, charts, graphs, and texts.
Results: among the 156 female sex workers (FSWs), 99 (63.5%) had been working on commercial sex for more than one year, 92 (59%) were usually street-based, and 80 (51.3%) had partners between 2-3 per night. Only, 17 (10.9%) respondents mentioned three and above ways of HIV/AIDS transmission and prevention methods. Less than two-thirds (64.1%) of FSWs used a condom with all partners. One hundred thirty-eight (88.5%) of participants were engaged in unsafe sexual practice at least once since their engagement in sex work. Majority of FSWs (85.3%)) believed that their occupation is hazardous and 145 (92.9%) reported that they were unhappy being a commercial sex worker. Regarding risk perception, 79 (50.64%) and 37 (23.7%) of respondents perceived their chances of contracting HIV/STIs to be high and moderate respectively.
Conclusion: Knowledge about HIV/STIs and magnitude of condom utilization were good. However, a high number of unsafe sex and unsatisfactory risk perception attitudes were observed. Thus, a collaborative effort is needed to create awareness regarding risk perception attitude and increase the level of their practice towards the prevention of unsafe sex.
Half of the worlds population suffers from infections including HIV/AIDS, hunger and unsustainable access to safe water and basic sanitation [1]. HIV/AIDS continues to be a major global public health problem, having claimed more than 35 million lives so far. At the end of 2017, there were approximately 36.9 million people living with HIV with 1.8 million people becoming newly infected and 940 000 people who died from HIV-related causes globally [2, 3]. Likewise, in 2015, there were 36.7 million people living with HIV, and 1.1 million deaths [4, 5]. The African region accounts for over 2/3rd of the global total of new HIV infections [2]. Sub-Saharan Africa has been the most seriously HIV stricken region, accounting for seventy-one percent of all new infections in adults and children globally [2, 6, 7]. Ethiopia is one of the country in the world that has the largest HIV/AIDS burdens and experiencing a ‘generalized’ HIV epidemic (epidemic defined as the HIV seroprevalence level amongst sexually active adults in the general population is greater than one percent) with an estimated 741,478 people living with HIV and 16,865 AIDS-related death in 2015 [8]. In the same year, in Dire Dawa administration city, adult (15+ years) HIV prevalence was 3.26 with 120 new HIV infection, 9,523 HIV positive population, 251 annual AIDS deaths and 3,690 total AIDS orphan [8]. Sex workers and their clients, men who have sex with men, people who inject drugs, people in prisons and other closed settings, and transgender people are key populations that are at increased risk of HIV irrespective of epidemic type or local context. This key populations often have legal and social issues related to their behavior that increase vulnerability to HIV and reduce access to testing and treatment programmes. In 2017, an estimated 47% of new infections occurred among key populations and their partners [2].
Furthermore, it is recognized that HIV seroprevalence is considerably above this level amongst female sex workers and mobile populations [9]. Female sex workers are the highly vulnerable groups that are at high risk of contributing to sexually transmitted diseases [10, 11]. Even though street-based female sex workers (FSWs) are highly vulnerable to HIV, only about one in every three of them receive adequate HIV prevention services and medical care [12, 13]. Female sex workers encountered numerous challenges from their clients that expose them to unsafe sex, because of their hazardous occupational situation [14-16]. Therefore, effective, consistent and correct utilization of condom is one of the best preventive intervention methods of HIV and others STIs targeted toward female sex workers. It would avert two-thirds of an incident of HIV infections [17-20]. Use of male and female condoms, increasing the availability, accessibility, and affordability of condom among female sex workers are an essential component to reduce the enormous consequences and costs of STIs and unintended pregnancies [1, 19]. Regardless of many efforts in the world, there is still no vaccine & cure for HIV/AIDS [2, 4]. However, effective antiretroviral drugs can control the virus & help prevent transmission so that people with HIV, & those at substantial risk, can enjoy healthy, long & productive lives [2]. Despite these, there is still a tangible and visible gap between the desired goal to achieve and the present level of condom utilization among FSWs [12, 21]. In addition, unsatisfactory and inadequate HIV and condom utilization knowledge and negative risk perception attitude are the challenges among female sex workers to fight HIV/STIs [22, 23]. Thus, this study assessed the level of female sex workers' HIV/AIDS knowledge, risk perception and condom utilization pattern in Dechatu, Dire Dawa, Eastern Ethiopia.
Study period and area: this study was conducted in Dire Dawa city from April 15-June 25, 2016. Dire Dawa is found 515km away from the capital city of Ethiopia, and 315km to Djibouti. The Population size was about 398,429 with 49% male and 51% female based on the 2007 Ethiopian census. The city has 9 urban and 38 rural Kebele with 54,575 urban and 22,240 rural households. Dechatu is one of kebele among the 9 urban kebele with the total population size of 22,205. It has 13 ketena that is bounded by Coneal in the east, Kezira from the North, Addisketma from the South and Legahara from the West. It has one public school, one private school, and one public health center.
Study design and participants: a cross-sectional study was conducted in Dire Dawa to assess female sex workers HIV/AIDS knowledge, risk perception, and condom utilization pattern. All female sex workers between the ages of 15-49 years living in the study area for at least 6 months were included for an interview but those who had a physical impairment (unable to hear and speak) and mentally ill were excluded from the study.
Sample size determination and technique: the sample size (n) required for the study was determined using a single population proportion formula
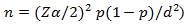
whereas n = the required sample size, Za/2(1.96): significance level at α=0.05 with 95% confidence interval, p: proportion of condom utilization among female sex workers (89.5%) [24], d: margin of error (5%) and 10% non-response rate. Therefore, the formula would provide the sample size of n=156. Convenient sampling method was used to recruit study participants as it was not possible to have a sampling frame for this population study, and their hidden and hard-to-reach behavior.
Measurement and data collection procedure: data was collected face to face using a pretested questionnaire that was adapted from different kinds of literature [25-27] and modified to suit the study objectives. It contains female sex workers' socio-demographic status, HIV/AIDS and condom knowledge, risk perception and condom utilization pattern. Three BSc nurses and 1 MSc nurse were selected for data collection and supervision respectively.
Data quality control: the data quality was assured by using different methods. The standard and structured questionnaire was used. The questionnaire was prepared in English and translated into the local language (Amharic) for data collection and then retranslated back into English for analysis. Two days of training was provided to the data collectors and supervisors on the data collection tool and the data collection procedures. Then the questionnaire was pretested on 5% of the sample size to ensure its validity. Findings from the pretesting were utilized for modifying and adjusting of the instrument and interviewing technique. Data collectors were supervised closely by the supervisors and the principal investigators. Completeness of each questionnaire was checked by the principal investigator and the supervisors on daylily basis. Double data entry was done by two data clerks and the consistency of the entered data was cross-checked by comparing the two separately entered data on Epi Info.
Data processing and analysis: after collection of the data, each questionnaire was thoroughly reviewed for completeness and consistency by the data collectors, supervisor and investigators. Then the data were entered into Epi Info version 3.1 and analyzed by using SPSS for window version 20. Descriptive statistics was employed to examine the findings using frequency, mean, mode and proportion. The results were presented using tables, charts, graphs, and result statements.
Ethics approval and consent to participate: the research proposal was ethically cleared by the Department Research and Ethical Review Committee (DREC) and approved by the school of nursing & midwifery, college of health and medical science, Haramaya University. Informed verbal consent, which was approved by ethics committee, was obtained from each study subject prior to the interview after the purpose of the study was explained to them. If the respondents were under 16, consent to participate was taken from the parental/legal guardian. Confidentiality of the information was assured and privacy of the respondent was maintained.
A total of number of 156 female sex workers were involved in the data collection with a 100% response rate. Therefore, 156 respondents' data were included in the analysis.
Sociodemographic characteristics of the respondents: half of the respondents (50%) were between the age group of 20-24 years old and 15-19 years (44.9%) with a mean age of 19.5 and the median age of 20. The mean and median age of the participants at first sex and first selling sex were 17 and 18 years and 20 and 19 years old respectively. Majority of the female sex workers (88.5%) were ever unmarried. Concerning the educational status of the respondents, less than half (44.2%) of the FSWs had attended from 5 to 8 grade, and nearly one-quarter of them (24.4%) were illiterate but none of the respondents attained higher education. Regarding, residence and employment, all of the FSWs reported that they were currently living in Dire Dawa town. Only 12% of them were involved in income generating activities other than sex work. From the total respondents, 51.3% were orthodox religion followers and the remaining were Muslim. Seventy-six (48.7%) of FSWs were from Amhara ethnicity (Table 1).
Usual place of respondents to pick up their clients: in relation to the place of female sex workers to pick their clients, 92 (59%) were usually street-based and the remaining 64 (41%) were bar/hotel based to get their partner for a single time or more than single moment (Figure 1).
Female sex workers (FSWs) engagement period, number of partners, average income: among the involved FSWs for an interview, 99 (63.5%) reported that they had been working on commercial sex for more than a year and 21 (13.5%) had been engaging in commercial sex for less than six months. We also asked them about their average number of partners per night. Accordingly, 80 (51.3%), 48 (30.8%) and 28 (18.0%) of them had between two and three partners, more than three partners and one partner per night respectively. Among those who had reported having more than three partners per night, 42 (87.5%) were street-based FSWs and the remaining 6 (12.5%) were bar/hotel based. Concerning their average income per night, 78 (50%) of FSWs had reported that they usually got fifty-one to eighty Ethiopian Birr per night (Table 2).
Female sex workers Knowledge about HIV/AIDS and Condom: regarding HIV/AIDS transmission and prevention methods, 149 (95.5%) of FSWs mentioned one method, 115 (73.7%) mentioned two methods and the remaining 17 (10.9%) mentioned three and above diffent methods of HIV/AIDS transmission and prevention. (Table 3). Female sex workers knowledge of condom was measured by asking about the ability of the condom to prevent HIV/AIDS and its availability, accessibility & affordability. Based on these, 138 (88.5%) of FSWs believed that condom can prevent HIV/AIDS. All of the respondents reported that condom is available in nearby their occupational area (such as shops, pharmacy, health facilities, and bars) but only 16.7% of them Obtained condom freely as they want and 75% of females obtained in reasonable cost (purchasing in the exchange of less than one Ethiopian birr per pack of condom) (Table 3).
Condom utilization pattern and associated sexual behaviors: regarding condom utilization, 140 (89.7%) of FSWs always used condoms, 100 (64.1%) used condoms with all partners, 9 (5.8%) used condoms as needed and 31 (19.9%) of them didn't use condoms with their regular partners during sexual intercourse (Figure 2). In contrast, one hundred and thirty-eight (88.5%) of the females, had been engaged in unsafe sexual practice at least once since their engagement in sex work. The main reason listed by them to engage in unsafe sex was due to deliberate acts of their partners (34.1%) like: lack of condom utilization skill by their partners (26.1%), paid beyond normal (12.3%), forced by their client (08.0%), alcohol intoxication (04.3%) and the rest didn't remember the reasons. Respondents ability to convincing their partners about unsafe sex was also unsuccessful. From those who were asked for unsafe sex by their partner at least once since their engagement of sex work, only 20% of them tried to convince their partner/client but the remaining (80%) couldn't. As a result, they quarreled and disagreed (Table 4). As like other variables, consistency in utilization of condom was also assessed. Among 140 (89.7%) FSWs who reported that they had used a condom, 100 (71.4%) of them used with all partners, 31 (22.1%) with their regular partners (‘lovers’) and 9 (6.4%) said that they had used as needed (Table 5).
Risk perception of female sex workers towards HIV and/or other Sexual transmitted infections: FSWs were asked about the hazards of commercial sex from the angles of its potency in exposing themselves to HIV/STIs. One hundred thirty-three (85.3%) of them stated that this occupation was hazardous, 15 (9.6%) hadn't had that much hazard and the remaining 8 (5.1%) said the occupation hadn't had any risk of exposing them to HIV/STIs. About the level of job satisfaction, 145 (92.9%) described that they were unhappy with the commercial sex, 5 (3.20%) reported that they were happy and the rest 6 (3.84%) said that they didn't know. The reason forwarded by those who had said ‘unhappy’ for their engagement in commercial sex was family conflict [84 (53.8%)], those who couldn't get another job were [38 (37.17%)], those who faced peer pressure were [10 (6.41%)] and those who did not know were [4 (2.56%)].
FSWs were also requested to rank their chances of becoming infected with HIV/STIs based on their past sexual and other risky behaviors. Consequently, 79 (50.64%), 37 (23.7%), 25 (16%), and 15 (9.61%) of respondents perceived their chances of contracting HIV to be high, moderate, low/nil respectively, and the remaining couldn't rank their chances contracting HIV/STIs infection. Respondents were also asked to give reasons for their personal perceived risk of HIV/STIs infection. The majority [65 (42%)] of FSWs who perceived their risk as high or moderate, said that they had encountered high failures with condoms during sexual practice and 36 (23%) said that they were forced to practice unsafe sex by persons whom they suspect for having HIV/STIs. On the other hand, those FSWs who perceived their risk of HIV infection as low or nil gave a common reason of being very condom concious [13 (8%)], those who had had only one partner with whom they practice unsafe sex were [7 (4.5%)] and the remaining [5 (3%)] said that they hadn't practiced sexual intercourse with a client whom they suspect or know has HIV.
The finding of this research revealed that most of the respondents (95.5%), knew at least one method of HIV/STIs transmission and prevention. This finding is significantly higher than a cross-sectional study conducted in Northwest Ethiopia [28]. The possible reason for the difference might be due to the expansion of media. Following these, there will be an increased awareness among female commercial sex workers about the transmission and prevention methods of HIV/STIs. In this study, 138 (88.5%) of FSWs believed that condom can prevent HIV/AIDS. This is in line with a study conducted in Arsi, Addis Ababa and Debre Berhan-Ethiopia (86%) [29] and Northwest Ethiopia ( 80.1%) [28]. The similarity of this finding could be due to the resemblance of socio-culture, the way of living of the FSWs and the nature of the work.
Condom utilization among female sex workers in this study (89.7%) is comparable with findings in Northwest Ethiopia (84.2%) [28] and Phnom Penh, Cambodia (86.9%) [30] but much higher than the studies conducted in Arsi, Addis Ababa and Debre Berhan-Ethiopia (33%) [29], Abidjan, Côte d´Ivoire (11%) [31], and Pretoria, South Africa (43%) [32]. The high promotion of condom use in the country and its access freely or at an affordable price may perhaps be the possible reasons for the differences. From the total, 138 (88.5%) of female sex workers were engaged in unsafe sexual practice at least once since their engagement in sex work. On the other hand, a study conducted in Metemma Yohannes, Northwest Ethiopia showed that [303 (63.9 %)] of FSWs engaged in unsafe sex [33]. The main reason to engage in unsafe sex might be due to deliberate acts of their partners, lack of condom utilization skill by their partners, paid beyond expected, forced by their client, and alcohol intoxication. From 140 (89.7%) of FSWs who reported that they had used a condom, 100 (71.4%) of them used a condom with all partners. This finding is lower than studies conducted in Savannakhet, Lao PDR (97%), Southern India, (85%), and Mekelle, Ethiopia (94.2%) [34-36]. On the other hand, it is higher than studies conducted in Northwest Ethiopia (47.7%), Arsi, Addis Ababa and Debre Berhan-Ethiopia (59%), Zhejiang province, China (50.5%), and Democratic Republic of Congo (40%) [28, 29, 37, 38]. The discrepancy might be due to the difference in geographical area, sample size, socio-economic and culture. FSWs were also asked about their average number of partners per night. Accordingly, 80 (51.3%) of the females had between two and three partners per night respectively. Unlike this, 64 (16.5%) FSWs had two or more sexual clients per day in Fenoteselam, Ethiopia [38]. The difference could be due to that the respondents in this study are living in a more urbanized and civilized city of the country compared to those living in Fenoteselam, Ethiopia.
In this study, 133 (85.3%) of FSWs believed that this occupation was hazardous and had a risk of exposing them to HIV, 79 (50.64%) and 37 (23.7%) of respondents perceived their chances of contracting HIV to be high and moderate respectively. On the opposite, 67%, 68% and 58% of FSWs in Addis Ababa, Debre Berhan Arsi-Hitosa-Ethiopia didn't feel vulnerable to HIV/AIDS respectively [29]. The educational background is the probable reasons for these difference. Regarding the level of job satisfaction, 145 (92.9%) reported that they were unhappy with the commercial sex and only 5 (3.20%) reported that they were happy. A cross-sectional survey conducted in Queensland, Australia among 247 female sex workers showed that most sex workers reported positive job satisfaction. The discrepancy may due to the payment difference and the care given by their sexual partner.
Knowledge about HIV/STIs and magnitude of condom utilization were good. However, a great number of female sex workers had engaged in unsafe sex and only half of them perceived that they have the probability of a high chance of contracting HIV/STIs. Thus, a collaborative effort is needed to create awareness among FSWs regarding risk perception attitude and increase the level of their practice towards the prevention of HIV/STIs and unsafe sex.
What is known about this topic
- Female sex workers are high-risk groups for the contraction and transmission of STIs/HIV;
- Female sex workers encountered numerous challenges from their clients that expose them to unsafe sex, because of their hazardous occupational situation;
- Effective, consistent and correct utilization of condom would avert two-thirds of an incident of HIV infections.
What this study adds
- Most female sex workers in the study setting mentioned condom as preventive method for STIs/HIV;
- An encouraging condom utilization was observed among female sex workers in the last six months during sexual intercourse with their partners;
- Majority of female sex workers have been engaged in unsafe sexual practice at least once since their engagement in sex work, mainly due to deliberate acts and lack of condom utilization skill by their partners.
The authors declare no competing interests.
HM had a substantial contribution from conception to the acquisition of data. All the authors had a great contribution to study design, analysis, and interpretation of the findings. HM drafted the manuscript. All authors revised the paper carefully for important intellectual contents. All authors read and approved the final manuscript.
The authors are grateful to Haramaya university for the chance of conducting this research. We would like to thank Dire Dawa city administration for giving us permission to conduct this research in town. Our sincere gratitude and appreciation to forward data collectors and participants without whom this study would not be realized.
Table 1: sociodemographic characteristics of FSWs in Dechatu, Diredawa, eastern Ethiopia 2016 (n=156)
Table 2: FWS’s engagement period, number of partners, average monthly income in Dire Dawa town, 2016 (n=156)
Table 3: knowledge of FSWs about HIV/AIDS transmission and prevention methods, Dechatu, Diredawa, eastern Ethiopia, 2016 (n=156)
Table 4: unsafe sexual practices and underline causes among female sex workers of Dechatu Diredawa, Ethiopia, 2016 (n=156)
Table 5: consistency utilization of condom among FSWs of Dechatu, Diredawa, Ethiopia, 2016 (n=156)
Figure 1: usual place of female sex workers to pick up their clients in Dechatu, Diredawa, eastern Ethiopia 2016 (n=156)
Figure 2: condom utilization pattern among female sex workers in Dechatu, Diredawa, eastern Ethiopia 2016 (n=156)
- World Health Organization. Global Health Observatory (GHO) data: World Health Statistics 2015: WHO; 2015. Accessed 21 February 2016.
- World Health Organization. HIV/AIDS: Key facts WHO2017. Accessed 19 July 2018.
- UNAIDS G. Global AIDS update 2016. Geneva, Switzerland: World Health Organization Library. 2016.
- Joint United Nations Programme on HIV/AIDS. Fact sheet 2015. Geneva, Switzerland: UNAIDS. 2015.
- HIV gov . Global HIV/AIDS Overview: The Global HIV/AIDS Epidemic 2016. Accessed 17 July 2018.
- World Health Organization, UNAIDS. AIDS epidemic update: December 2009: Regional Office Europe: WHO; 2009.
- Who U, Unicef. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva: UNAIDS. 2013;3-5.
- Ethiopian Federal HIV/AIDS Prevention and Control Office (HAPCO). HIV Epidemic Estimates by regional states and Ethiopia, 2015: Addis Ababa, Ethiopia; 2015
- Mitike G, Lemma W, Berhane F, Ayele R, Assefa A. HIV/AIDS Behavioral Surveillance Survey (BSS) Ethiopia 2002. Round one. 2002. Google Scholar
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Infectious diseases. 2012;12(7):538-49. PubMed | Google Scholar
- Mbirimtengerenji ND. Is HIV/AIDS epidemic outcome of poverty in sub-saharan Africa?. Croatian medical journal. 2007;48(5):605-17. PubMed | Google Scholar
- Surratt HL, O'Grady C, Kurtz SP, Levi-Minzi MA, Chen M. Outcomes of a behavioral intervention to reduce HIV risk among drug-involved female sex workers. AIDS and behavior. 2014;18(4):726-39. PubMed | Google Scholar
- Organization WH. UNAIDS: Global Report: UNAIDS report on the global AIDS epidemic. Geneva: WHO. 2010.
- Mitike G. HIV/AIDS behavioral surveillance survey (BSS) Ethiopia 2006: Round two2006.
- Organization WH. Guidelines for the management of sexually transmitted infections in female sex workers. Manila: WHO Regional Office for the Western Pacific; 2002. Google Scholar
- Mbugua N, Bukusi EA, Wagura A, Ngugi E. P6 14 Determinants of condom use among female sex workers in kenya: a case-crossover analysis. BMJ Publishing Group Ltd. 2017. Google Scholar
- Morris CN, Ferguson AG. Estimation of the sexual transmission of HIV in Kenya and Uganda on the trans-Africa highway: the continuing role for prevention in high risk groups. Sexually transmitted infections. 2006;82(5):368-71. PubMed | Google Scholar
- WHO. WHO Guidelines Approved by the Guidelines Review Committee. Consolidated Guidelines on HIV Prevention, Diagnosis, Treatment and Care for Key Populations-2016 Update. WHO Guidelines Approved by the Guidelines Review Committee. Geneva: World Health Organization Copyright (c) World Health Organization 2016.; 2016.
- Organization WH. Guidelines: prevention and treatment of HIV and other sexually transmitted infections among men who have sex with men and transgender populations: recommendations for a public health approach 2011. 2011.
- Organization WH. Consolidated guidelines on general HIV care and the use of antiretroviral drugs for treating and preventing HIV infection: recommendations for a public health approach. Geneva: World Health Organization. 2013:269.
- Buckingham R, Meister E, Webb N. Condom use among the female sex worker population in Thailand. International journal of STD & AIDS. 2004;15(3):210-1. PubMed | Google Scholar
- Lau JT, Tsui HY, Siah PC, Zhang KL. A study on female sex workers in southern China (Shenzhen): HIV-related knowledge, condom use and STD history. AIDS care. 2002;14(2):219-33. PubMed | Google Scholar
- Ankomah A, Omoregie G, Akinyemi Z, Anyanti J, Ladipo O, Adebayo S. HIV-related risk perception among female sex workers in Nigeria. HIV/AIDS (Auckland, NZ). 2011;3:93-100. PubMed | Google Scholar
- Alem A, Kebede D, Mitike G, Lemma W. Unprotected sex, sexually transmitted infections and problem drinking among female sex workers in Ethiopia. Ethiopian Journal of Health Development. 2006;20(2):93-8. Google Scholar
- Tamene MM, Tessema GA, Beyera GK. Condom utilization and sexual behavior of female sex workers in Northwest Ethiopia: A cross-sectional study. The Pan African medical journal. 2015;21:50-. PubMed | Google Scholar
- Lammers J, van Wijnbergen SJ, Willebrands D. Condom use, risk perception, and HIV knowledge: a comparison across sexes in Nigeria. HIV AIDS (Auckl). 2013 Oct 21;5:283-93. PubMed | Google Scholar
- Chariyeva Z, Colaco R, Maman S. HIV risk perceptions, knowledge and behaviours among female sex workers in two cities in Turkmenistan. Global public health. 2011;6(2):181-92. PubMed | Google Scholar
- Consultants UM. Factors Affecting Accessibility And Utilization Of Condom (A Community Based Study) The Futures Group International-Ethiopia. 2000. Google Scholar
- Bui TC, Markham CM, Tran LT, Beasley RP, Ross MW. Condom negotiation and use among female sex workers in Phnom Penh, Cambodia. AIDS and behavior. 2013;17(2):612-22. PubMed | Google Scholar
- Ghys et al. Increase in condom use and decline in HIV and sexually transmitted diseases among female sex workers in Abidjan, Cote d'Ivoire, 1991-1998, Mastro TD AIDS (London, England). 2003;17 Suppl 4:S121-2. PubMed | Google Scholar
- Wechsberg WM, Luseno WK, Kline TL, Browne FA, Zule WA. Preliminary findings of an adapted evidence-based woman-focused HIV intervention on condom use and negotiation among at-risk women in Pretoria, South Africa. Journal of prevention & intervention in the community. 2010;38(2):132-46. PubMed | Google Scholar
- Gezie LD, Taye BW, Ayele TA. Time to unsafe sexual practice among cross-border female sex workers in Metemma Yohannes, North West Ethiopia. BMC Public Health. 2015;15(1):710. PubMed | Google Scholar
- Andrews CH, Faxelid E, Sychaerun V, Phrasisombath K. Determinants of consistent condom use among female sex workers in Savannakhet, Lao PDR. BMC Womens Health. 2015 Aug 19;15:63. PubMed | Google Scholar
- Vejella S, Patel SK, Saggurti N, Prabhakar P. Community Collectivization and Consistent Condom Use Among Female Sex Workers in Southern India: Evidence from Two Rounds of Behavioral Tracking Surveys. AIDS Behav. 2016;20(4):776-87. PubMed | Google Scholar
- Weldegebreal R, Melaku YA, Alemayehu M, Gebrehiwot TG. Unintended pregnancy among female sex workers in Mekelle city, northern Ethiopia: a cross-sectional study. BMC Public Health. 2015 Jan 31;15:40. PubMed | Google Scholar
- Ma Q, Jiang J, Pan X, Cai G, Wang H, Zhou X, et al. Consistent condom use and its correlates among female sex workers at hair salons: a cross-sectional study in Zhejiang province, China. BMC Public Health. 2017;17(1):910. PubMed | Google Scholar
- Kayembe PK, Mapatano MA, Busangu AF, Nyandwe JK, Musema GM, Kibungu JP, et al. Determinants of consistent condom use among female commercial sex workers in the Democratic Republic of Congo: implications for interventions. Sexually transmitted infections. 2008;84(3):202-6. PubMed | Google Scholar
- Anteneh ZA, Agumas YA, Tarekegn M. Sexually transmitted diseases among female commercial sex workers in Finote Selam town, northwest ethiopia: a community-based cross-sectional study. HIV AIDS (Auckl). 2017 Mar 2;9:43-49. PubMed | Google Scholar













