Ventricular restoration in adults with huge congenital left ventricular aneurysm: report of two cases
Charles Mve Mvondo, Hermann Nestor Tsague Kengni, Laurence Carole Ngo Yon, Amalia Ariane Owona Ngandebe, Etienne Sene, Marcelin Ngowe Ngowe
Corresponding author: Charles Mve Mvondo, Division of Cardiac Surgery, Shisong Cardiac Centre, Kumbo, Cameroon 
Received: 28 Aug 2022 - Accepted: 02 May 2024 - Published: 06 May 2024
Domain: Cardiovascular surgery
Keywords: Congenital aneurysm, ventricular restoration, Cameroon, case report
©Charles Mve Mvondo et al. Pan African Medical Journal (ISSN: 1937-8688). This is an Open Access article distributed under the terms of the Creative Commons Attribution International 4.0 License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cite this article: Charles Mve Mvondo et al. Ventricular restoration in adults with huge congenital left ventricular aneurysm: report of two cases. Pan African Medical Journal. 2024;48:8. [doi: 10.11604/pamj.2024.48.8.36988]
Available online at: https://www.panafrican-med-journal.com//content/article/48/8/full
Case report 
Ventricular restoration in adults with huge congenital left ventricular aneurysm: report of two cases
Ventricular restoration in adults with huge congenital left ventricular aneurysm: report of two cases
![]() Charles Mve Mvondo1,2,&, Hermann Nestor Tsague Kengni2,
Charles Mve Mvondo1,2,&, Hermann Nestor Tsague Kengni2, ![]() Laurence Carole Ngo Yon2, Amalia Ariane Owona Ngandebe3, Etienne Sene4,
Laurence Carole Ngo Yon2, Amalia Ariane Owona Ngandebe3, Etienne Sene4, ![]() Marcelin Ngowe Ngowe2
Marcelin Ngowe Ngowe2
&Corresponding author
Congenital ventricular aneurysms (CVA) are rare cardiac anomalies that have been predominantly described in the Black population. They are characterized by an akinetic ventricular protrusion that is commonly located at the basal and apical segments. Although the diagnosis is often incidental and the majority of patients are asymptomatic, life-threatening events such as persistent ventricular arrhythmias, CVA rupture, and heart failure are not uncommon. However, no standardized therapy is currently available and good outcomes have been reported with both conservative and surgical management. We report the cases of two young Black African patients with huge symptomatic CVA lesions who underwent successful surgical repair with a ventricular restoration technique. Both cases were consulted for chest pain and dyspnea. Chest X-ray and transthoracic Doppler echocardiography suggested the diagnosis. Thoracic angioscanner and thoracic magnetic resonance imaging confirmed the diagnosis. Both patients underwent successful surgery. This case report aims to revisit the diagnostic and therapeutic approach to this rare pathology, in our professional environment.
Congenital ventricular aneurysms (CVA) are rare entities with an estimated incidence between 0.02% and 0.34% [1,2]. The CVA appears as a saccular and akinetic extension of the ventricular wall, mainly located at the apical segment in the majority [2]. The left ventricle is the mostly affected, and the differential diagnoses are with congenital ventricular diverticula (CVD) and acquired ventricular aneurysms such as post-myocardial infarction aneurysms and infectious conditions such as viral cardiomyopathy and myocardial involvement in Chagas and tuberculosis diseases [3-6]. Despite the risk of life-threatening complications such as rupture, there has been some reluctance to recommend surgical therapy unless symptoms are present or in cases with associated cardiac lesions. We report the cases of two young adults who underwent ventricular restoration for symptomatic and complicated CVA in our institution. This case report aims to revisit the diagnostic and therapeutic approach to this rare pathology, in our professional environment.
Case 1
Patient information: a 27-year-old Black male patient was referred to our department from an outside hospital with a diagnosis of a large apical ventricular pseudo-aneurysm. The patient had no familial history of cardiovascular disease or sudden death.
Clinical findings: he complained 3 weeks earlier of recurrent headaches, general body weakness, thoracic compression, and sporadic episodes of palpitations.
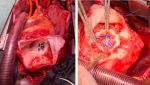
Diagnostic assessment: the electrocardiogram showed a Cornell index at 28 mm with ST-T changes in leads V5 and V6. While a Color-Doppler transthoracic echocardiogram ruled out valvular, congenital, and ventricular dysfunction, an apical flow acceleration was found with a suspicion of left ventricular diverticulum or aneurysm. The latter was confirmed at subsequent Magnetic Resonance Imaging (MRI) describing an akinetic fibrotic and partially thrombosed cavity, suggesting an apical CVA (Figure 1), communicating with the left ventricle through a 2-centimetre defect. Additional investigations with 24-hour Holter-Electrocardiogram, chest X-ray, and serology (VDRL, HIV) did not reveal other abnormalities.
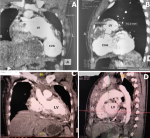
Therapeutic interventions: an oral anticoagulation prophylaxis and beta-blocker therapy were initiated with poor improvement of the symptoms after 3 weeks of treatment. Following a clinical discussion with the following cardiologist and the patient, a consensual decision was taken for elective surgical repair. The patient underwent a successful ventricular restoration with a bovine pericardial patch under cardiopulmonary bypass (Figure 2).
Follow-up and outcome of interventions: the postoperative course was uneventful and the patient was discharged from the hospital 6 days after surgery.Informed consent: the patient reported his full consent to publish his case.
Case 2
Patient information: a 29-year-old woman with a known history of thoracic mass was admitted to the emergency department of our institution for progressive tachypnea.
Clinical findings: she complained two months earlier of recurrent thoracic compression and dyspnea.
Diagnostic assessment: a chest X-ray revealed left para-cardiac opacity without parenchymal involvement. The electrocardiogram showed a first-degree atrioventricular block, left ventricular hypertrophy with a Cornell index at 27 mm, Cornell product criteria at 3240mVms, and ST-T changes in leads V5 and V6. An emergency angio-computed tomography scan revealed a huge thrombosed cavity communicating with the left ventricle at the apical segment (Figure 3).
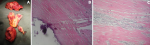
Therapeutic interventions: considering the risk of rupture, an urgent surgery was planned. A diagnosis of large CVA was made intra-operatively and the patient underwent a surgical ventricular restoration and mass resection (Figure 4).
Follow-up and outcome of interventions: the postoperative course was uneventful and the patient was discharged home on the 10th postoperative day. A postoperative angio-computed tomography scan showed no residual shunt and good restoration of the left ventricular shape (Figure 3).
Informed consent: the patient reported her full consent to publish her case.
CVA lesions are a large spectrum of heterogeneous patterns varying from isolated myocardial protrusions, described mostly in autopsy studies, to voluminous protuberances as observed in the current series. While the precise mechanism of CVA development remains unknown, embryogenic defects within the endocardial tube from the 4th embryogenic week have been hypothesized [7]. No evidence of sex predominance is supported by various reports, while the majority of CVA patients were mainly from African and American regions [2]. Morphologically, CVAs appear as akinetic and fibrous protuberances of the ventricular wall, with a predominant location at the apical segment [1, 2]. They are histologically distinct from congenital ventricular diverticula (CVD) which wall presents intrinsic similarities with myocardial tissue, including contractile activity. As opposed to CVA, CVD is commonly associated with cardiac and/or extra-cardiac lesions [8]. Other differential diagnoses are post-infarction ventricular aneurysms and aneurysmal lesions from infectious processes such as the human immunodeficiency virus, Chagas, and tuberculosis diseases [3-6]. The heterogeneity of CVA lesions, with regards to size, location, thrombosis, and associated anomalies, translates in a variety of clinical presentations from asymptomatic status which is the majority, to more invaliding events such as persistent arrhythmias, heart failure, rupture, and sudden death [9].
The diagnosis of CVA is often incidental during routine investigations for other diseases. Although CVA can be associated with electrical abnormalities [10], these events are relatively rare [11]. Pellicia et al. suggested a classification in 3 groups (distinct, mild, and minor) of these electrocardiographic abnormalities [12]. According to that classification, the abnormalities observed were then mild although the sensitivity, specificity, positive predictive value, and negative predictive value of a 12-lead ECG for the diagnosis of CVA are low [11]. CVA lesions can be primarily detected by Color-Doppler Echocardiography which is largely accessible and provides a reliable description of ventricular morphology and associated cardiac anomalies, despite misdiagnoses of small apical lesions are possible [13,14]. Complementary imaging with Magnetic Resonance Imaging (MRI), computed tomography Scan, and conventional computed angiography is often required in doubtful cases and when surgical correction is considered. They provide specific details on CVA tissue, size, kinesia (to differentiate CVA from CVD), and associated lesions such as congenital anomalies in children and/or coronary disease in adult patients [15,16]. To date, no consensus exists in clinical practice for the management of CVA due to its scarce prevalence. Indeed, limited data from case series have presented heterogeneous outcomes with several strategies including surgical repair, antiarrhythmic treatment, and conservative management among others [2,9]. In a study by Mayer et al., no cardiac death was observed among patients with CVA and CVD who underwent conservative management over a 13-year follow-up period [17]. Similar experiences with non-surgical approaches were reported by other authors with imaging follow-up from the fetal period [18,19]. However, surgery was mostly described in cases with associated anomalies or those with clear symptoms, following congestive heart failure, thromboembolism, and sustained ventricular arrhythmias. The type of surgery depends on the size and location of the CVA, in addition to the associated anomalies. Simple direct suturing of small defects (<2 cm) is often sufficient, whereas larger lesions require more complex procedures such as ventricular restoration with circular patches as described in post-infarction ventricular aneurysm surgery [1,20]. Thus, care should be taken to avoid restrictive dysfunction following ventricular repairs, and mitral valve insufficiency resulting from displacement/distortion of the papillary muscles. If the operative risk is relatively low (<2%) in isolated lesions, it might significantly increase in cases with associated anomalies. In our case, the repair of a giant thrombosed CVA with partial rupture required femora-femoral cannulations for cardiopulmonary bypass and moderate hypothermia considering the risk of complete rupture during chest entry. In cases presenting with ventricular sustained arrhythmias, antiarrhythmic treatment including radiofrequency ablation or ICD implantation has been described as lone therapy or in combination with surgery [21,22].
Fatal complications from CVA could be more common than expected. Thus, an accurate evaluation of ventricular wall abnormalities during routine imaging analysis should be considered in patients presenting with symptoms of heart failure, stroke, and ventricular arrhythmias. Surgical treatment is effective and should be considered in cases refractory to conservative therapy.
The authors declare no competing interests.
Patient management: Charles Mve Mvondo, Hermann Nestor Tsague Kengni, Laurence Carole Ngo Yon, Amalia Ariane Owona Ngandebe, and Etienne Sene. Data collection: Charles Mve Mvondo, Hermann Nestor Tsague Kengni and Laurence Carole Ngo Yon. Manuscript drafting: Charles Mve Mvondo, Hermann Nestor Tsague Kengni, and Laurence Carole Ngo Yon. Manuscript revision: Charles Mve Mvondo, Hermann Nestor Tsague Kengni, Laurence Carole Ngo Yon, Amalia Ariane Owona Ngandebe, Etienne Sene, and Marcelin Ngowe Ngowe. All authors read and approved the final version of the manuscript.
Figure 1: left apical congenital ventricular aneurysms at magnetic resonance imaging (A, B)
Figure 2: intraoperative views of the congenital ventricular aneurysms, A) apical defect, B) closure of the defect with a bovine pericardium
Figure 3: angio-computed tomography scan views: comparative aspects, preoperative (A, B), postoperative (C, D)
Figure 4: excised congenital ventricular aneurysms with diffused thrombosis (A), histopathology of congenital ventricular aneurysms wall (B, C) showing fibrotic tissue with diffused inflammatory cells and focus of calcification
- Ohlow MA, Secknus MA, Geller JC, Von Horn H, Lauer B. Prevalence and outcome of congenital left ventricular aneurysms and diverticula in an adult population. Cardiology, vol. 2009;112(4):287-293. PubMed | Google Scholar
- Ohlow MA, Von Horn H, Lauer B. Characteristics and outcomes of congenital left ventricular aneurysms and diverticula: analysis of 809 cases published since 1816. Int J of Cardiology. 2015;185:34-45. PubMed | Google Scholar
- McDicken I, Groden BM, James WB. Cardiac aneurysm after myocardial infarction. Postgrad Med J. 1968;44:75-84. PubMed | Google Scholar
- Oliveira JS, Mello De Oliveira JA, Frederigue U Jr, Lima Filho EC. Apical aneurysms of Chagas heart disease. Br Heart J. 1981;46:432-437. PubMed | Google Scholar
- Jones KP, Tilden K. Tuberculous myocardial aneurysm with rupture and sudden cardiac death from tamponade: review of the literature and report of a case. Hawaii Med J. 1942;1:295-297. Google Scholar
- Kane A, Hane L, Dangou JM, Diop IB, Thiam S et al. Anévrisme ventriculaire gauche au cours de l'infection par le virus de l'immuno-déficience humaine: à propos d'une observation [Left ventricular aneurysm in human immunodeficiency virus infection: a case report]. Arch Mal Coeur Vaiss. 1998 Apr;91(4):419-23. Google Scholar
- Van Mierop L, Kutschke L. Embryology of the heart. Hurst´s the heart. 8th edition. McGraw-Hill. 1994.
- Ohlow MA. Congenital left ventricular aneurysms and diverticula-Definition, pathophysiology, clinical relevance and treatment. Cardiology 2006; 106: 63-72. Google Scholar
- Ohlow MA. Congenital left aneurysms and diverticula: an entity in search of an identity. Journal of Geriatric Cardiology. 2017;14:750-762. PubMed | Google Scholar
- Shan S, He X, He L, Wang M, Liu C. Coexistence of congenital left ventricular aneurysm and prominent left ventricular trabeculation in a patient with LDB3 mutation: a case report. J Med Case Rep. 2017 Aug 19;11(1):229. doi: 1186/s13256-017-1405-1. PubMed | Google Scholar
- Ohlow, Marc-Alexander Lauer, Bernward Geller, J Christoph. Prevalence and spectrum of abnormal electrocardiograms in patients with an isolated congenital left ventricular aneurysm or diverticulum. EP Europace. 2009;11:1689-1695. Google Scholar
- Pelliccia A, Culasso F, Di Paolo FM, Accettura D, Cantore R, Castagna W et al. Prevalence of abnormal electrocardiograms in a large, unselected population undergoing pre-participation cardiovascular screening. Eur Heart J. 2007 Aug;28(16):2006-10. PubMed | Google Scholar
- Takahashi M, Nishikimi T, Tamano K, Hara S, Kobayashi T et al. Multiple left ventricular diverticula detected by second harmonic imaging: a case report. Circ J. 2003 Nov;67(11):972-4. PubMed | Google Scholar
- Hajsadeghi S, Pazoki M, Talebitaher M, Iranpour A. Giant congenital left ventricular diverticulum associated with infective endocarditis: A diagnosis made by tissue Doppler echocardiography. J Cardiol Cases. 2016 Aug 8;14(4):127-129. PubMed | Google Scholar
- Beregi JP, Aumégeat V, Coullet JM, DeGroote P, Debacker-Steckelorom C, Ducloux G. Case report: congenital left ventricular aneurysm diagnosed by spiral CT angiography. J Comput Assist Tomogr. 1996 May-Jun;20(3):484-6. PubMed | Google Scholar
- Sharma A, Kumar S. Overview of left ventricular outpouchings on cardiac magnetic resonance imaging. Cardiovasc Diagn Ther. 2015;5:464-470. PubMed | Google Scholar
- Mayer K, Candinas R, Radounislis C, Jenni R. Kongenitale linksventrikuläre Aneurysmen und Divertikel: Klinik, Diagnostik und Verlauf [Congenital left ventricular aneurysms and diverticula: clinical findings, diagnosis and course]. Schweiz Med Wochenschr. 1999 Sep 4;129(35):1249-56. Google Scholar
- Brachlow A, Sable C, Smith S, Slack M, Martin G. Fetal diagnosis and postnatal follow-up of an asymptomatic congenital left ventricular diverticulum. Pediatr Cardiol. 2002 Nov-Dec;23(6):658-60. PubMed | Google Scholar
- Cavallé-Garrido T, Cloutier A, Harder J, Boutin C, Smallhorn JF. Evolution of fetal aneurysms and diverticula of the heart: an echocardiographic study. Am J Perinatol. 1997;14:393-400. PubMed | Google Scholar
- Ruzza A, Czer LSC, Arabia F, Vespignani R, Esmailian F, Cheng W et al. Left Ventricular Reconstruction for Postinfarction Left Ventricular Aneurysm: Review of Surgical Techniques. Tex Heart Inst J. 2017 Oct 1;44(5):326-335. PubMed | Google Scholar
- Ouyang F, Antz M, Deger FT, Bänsch D, Schaumann A, Ernst S et al. An underrecognized subepicardial reentrant ventricular tachycardia attributable to left ventricular aneurysm in patients with normal coronary arteriograms. Circulation. 2003 Jun 3;107(21):2702-9. PubMed | Google Scholar
- Ogawa M, Miyoshi K, Morito N, Kodama S, Yahiro E, Fujimi K et al. Successful catheter ablation of ventricular tachycardia originating from the idiopathic saccular apical left ventricular aneurysm. Int J Cardiol. 2004 Feb;93(2-3):343-6. PubMed | Google Scholar